Einführung
Clinical trials face mounting pressure: rising costs, recruitment stagnation, and demands for faster, more accurate outcomes. AI is emerging as a game‑changer, automating patient matching, streamlining trial design, and predicting risks in real time.
This comprehensive guide explores how AI is revolutionizing clinical trials – unpacking use cases, tangible benefits, and implementation challenges.
Was ist KI und warum ist sie wichtig in Clinical Trials?

Definition of AI and Its Core Technologies
Artificial Intelligence (AI) refers to the development of computer systems that can perform tasks typically requiring human intelligence, such as reasoning, learning, and problem-solving. These systems rely on technologies like machine learning, natural language processing (NLP), and computer vision to process and analyze complex data. By identifying patterns and making predictions, AI enables faster and more accurate decision-making in data-rich environments.
In clinical trials, AI plays a critical role in automating processes that have traditionally been time-consuming and error-prone. It helps researchers streamline trial design, match patients more effectively, and analyze vast datasets with greater precision. This integration of AI enhances efficiency, reduces trial costs, and accelerates the path to regulatory approval.
The Growing Role of AI in Transforming Clinical Trials
AI is reshaping clinical trial operations by optimizing everything from design to execution. Machine learning models simulate trial outcomes in advance, helping researchers refine protocols early. This reduces delays and lowers the risk of costly amendments.
Natural language processing speeds up patient recruitment by analyzing health records and physician notes to find eligible participants. This improves matching accuracy and reduces enrollment time, a frequent barrier in trial execution. In some cases, platforms now reach over 90 percent accuracy.
Computer vision brings consistency to medical image analysis, surpassing human variability. Regulatory agencies are beginning to approve AI tools for evaluating trial endpoints. These technologies are raising the bar for reliability and efficiency in clinical assessments.
Key Statistics and Trends Highlighting AI Adoption in Clinical Trials
The global AI-in-clinical-trials market is projected to grow from USD 2.04 billion in 2024 to USD 22.36 billion by 2034, with a CAGR of 27%. North America currently holds the largest market share, accounting for about 40% of global revenue. This rapid growth reflects increasing investment in AI-driven optimization across the clinical development pipeline.
AI tools are already improving key metrics. McKinsey reports that AI can increase patient enrollment by 10–20% and significantly reduce trial cycle times. TrialMatchAI, an oncology-specific system, achieved 92% match accuracy within top recommendations and over 90% accuracy in eligibility classification.
By 2030, it’s expected that 60–70% of trials will integrate AI for tasks like design, recruitment, and monitoring, potentially saving the industry USD 20–30 billion annually. Adoption is being driven by improved data access, stronger algorithms, and the need for operational efficiency. These trends position AI as a core pillar of future clinical trial infrastructure.
Business Benefits of AI in Clinical Trials
AI is delivering measurable value across every stage of the clinical trial process. From faster study design to safer monitoring, it addresses longstanding inefficiencies and enhances trial performance at scale.
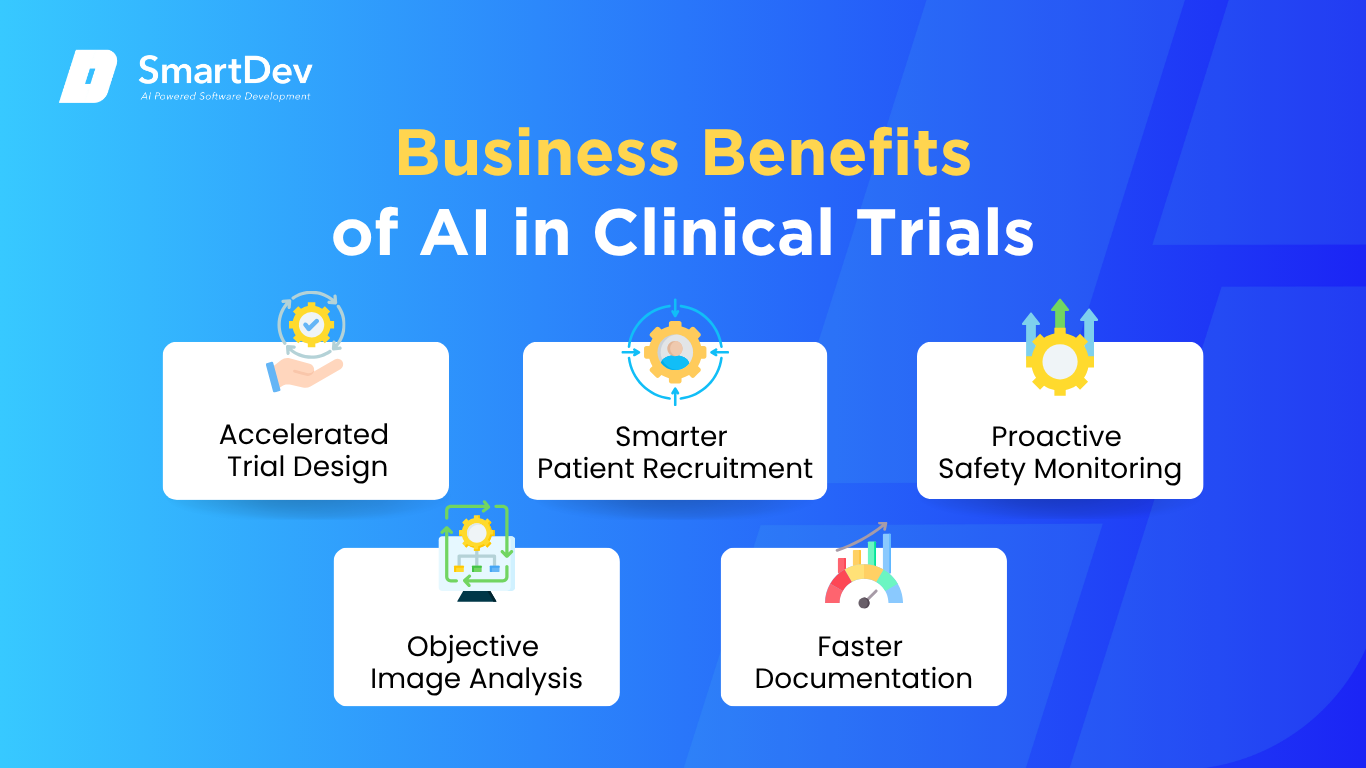
1. Accelerated Trial Design
AI enables researchers to model and refine trial protocols before patient enrollment begins. This reduces delays and the likelihood of costly amendments. As a result, trials can move from design to launch more efficiently.
Adaptive tools can modify protocols in real time based on interim findings. This flexibility improves both trial outcomes and resource use. Sponsors benefit from more efficient study execution and reduced operational risk.
2. Smarter Patient Recruitment
AI analyzes large volumes of clinical data to identify eligible participants with greater speed and accuracy. This shortens enrollment periods and improves match quality. Recruitment becomes more efficient and less reliant on manual screening.
These systems can also support more diverse and representative participant selection. Broader recruitment improves the validity of clinical results and regulatory acceptance. Trials benefit from faster completion and higher data quality.
3. Proactive Safety Monitoring
AI continuously evaluates incoming trial data to detect potential safety issues early. This allows teams to respond quickly and protect participant well-being. Early detection reduces disruptions and supports more stable trial progression.
These systems improve their accuracy over time through ongoing data analysis. Unlike static methods, AI adapts to real-world variability in patient responses. This makes safety monitoring more responsive and reliable.
4. Objektiv Image Analysis
AI tools provide consistent, automated analysis of medical images used in clinical endpoints. This minimizes interpretation variability and strengthens data reliability. Standardized image assessment contributes to clearer outcome measures.
By automating image review, these tools also reduce workload and speed up data processing. Consistency in analysis supports better regulatory and clinical decision-making. Trials benefit from higher accuracy and reproducibility.
5. Faster Documentation
AI can automate the drafting of protocols, forms, and regulatory documents based on trial requirements. This reduces manual workload and accelerates preparation timelines. Teams can focus more on review and compliance.
These tools help maintain consistency across documentation and align with regulatory standards. Automation also reduces the risk of human error. Overall, trial documentation becomes faster, more accurate, and easier to manage.
Herausforderungen bei der Einführung von KI in Clinical Trials
Despite its promise, AI adoption in clinical trials comes with real-world barriers. These challenges span regulatory gaps, data quality issues, and ethical concerns that organizations must address to ensure safe and effective implementation.
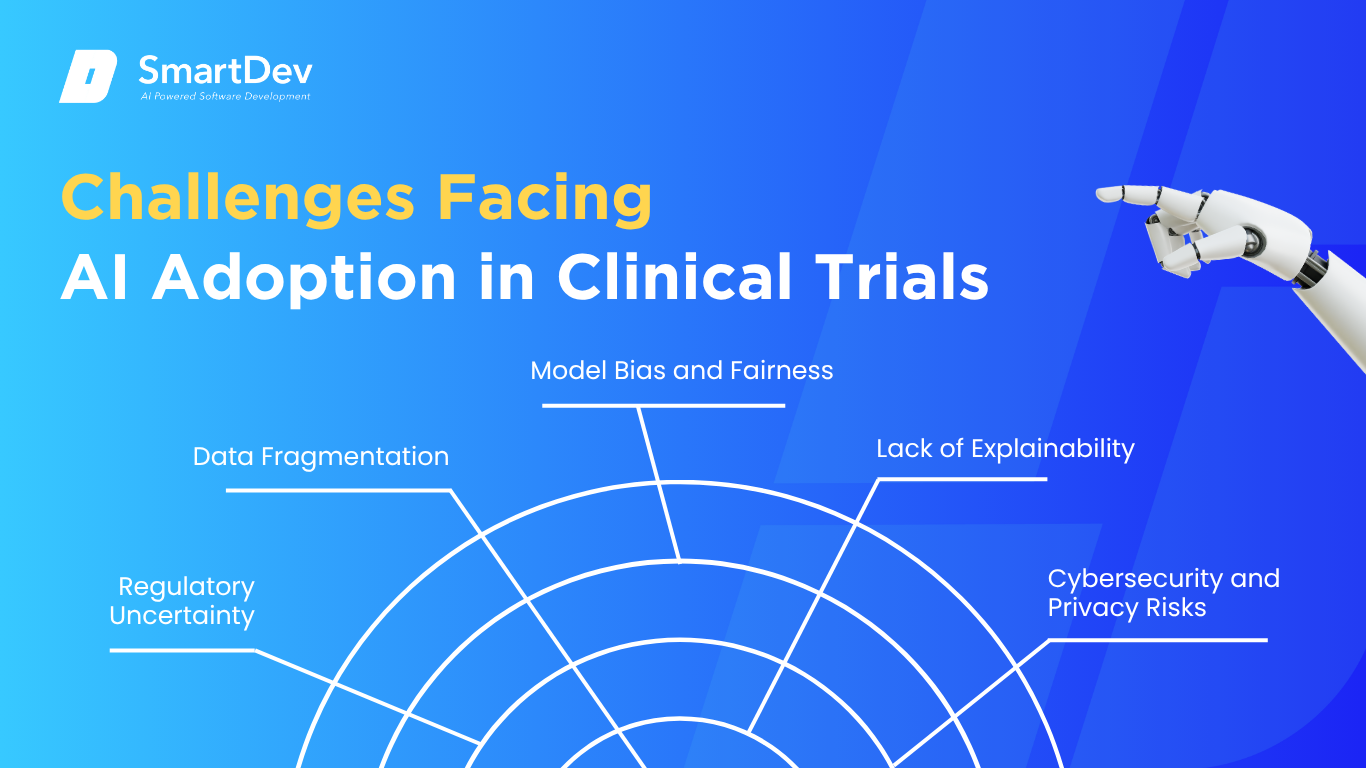 1. Regulatory Uncertainty
1. Regulatory Uncertainty
AI tools in clinical trials often operate ahead of established regulatory frameworks. Lack of clear guidance on validation, transparency, and auditability can slow adoption. Sponsors may hesitate to invest without assurance of compliance and approval pathways.
Regulators are working to adapt, but progress varies by region and application type. Until consistent standards emerge, uncertainty will remain a barrier. Developers must build systems that prioritize explainability and traceability from the start.
2. Data Fragmentation
Clinical data is often spread across incompatible systems, formats, and sources. This fragmentation makes it difficult for AI models to access the clean, structured data they need. As a result, model performance can suffer and insights may be unreliable.
Integrating data from electronic health records, lab systems, and trial platforms requires significant effort. Without standardized data pipelines, scaling AI solutions becomes complex. Investment in data infrastructure is essential to realize AI’s full value.
3. Model Bias and Fairness
AI models trained on limited or non-representative datasets can produce biased outputs. This poses serious risks in patient selection and outcome prediction. Unchecked bias can compromise trial integrity and undermine trust in results.
Addressing this requires diverse data inputs and continuous model auditing. Fairness must be embedded in both development and deployment processes. Ensuring equity in AI systems is critical for ethical and scientific standards.
4. Lack of Explainability
Many AI models, especially in deep learning, function as “black boxes” with limited insight into how decisions are made. This lack of transparency can reduce trust among clinicians, regulators, and trial sponsors. It also complicates the validation of AI-derived conclusions.
Explainable AI frameworks aim to bridge this gap, but they are still evolving. Balancing performance with interpretability remains a key challenge. Stakeholders require clear, auditable reasoning for AI outputs to gain confidence in the results.
5. Cybersecurity and Privacy Risks
AI systems in clinical trials handle sensitive patient data across digital platforms. This increases exposure to cyber threats, data breaches, and misuse. A single breach can jeopardize patient trust and regulatory standing.
Ensuring compliance with data protection laws requires robust encryption, access controls, and audit trails. As AI adoption expands, so does the need for advanced security protocols. Continuous monitoring and secure architecture are essential to protect trial integrity.
Explore how AI enhances digital resilience in our guide to strategic cyber defense against modern threats.
Specific Applications of AI in Clinical Trials

1. AI‑Driven Patient Recruitment
AI models streamline patient identification by analyzing EHRs, claims, and demographic data to match individuals to trial criteria. NLP parses unstructured notes, lab results, and clinical narratives to uncover eligibility signals beyond diagnostic codes. Predictive analytics then prioritize candidates with high likelihood of enrollment and retention, integrating seamlessly into trial management platforms.
This yields faster enrollment, improved matching quality, and lower recruitment costs – critical for meeting tight trial timelines. Moreover, AI enhances diversity by uncovering underrepresented subgroups from large datasets. Ethical safeguards like HIPAA/GDPR compliance and transparent model validation are essential to protect patient privacy and trust.
Integration involves embedding algorithms into CRO dashboards or EHR tools, with feedback loops refining models based on enrollment outcomes. Teams must monitor bias (e.g., underrepresentation of certain ethnicities) and ensure models generalize across sites. Regular auditing and human oversight balance efficiency with ethical rigor.
Real-world example:
IQVIA’s AI-powered patient recruitment improved target patient identification by 15× and healthcare provider linkage by 10×, resulting in a 28% treatment initiation rate within three months.
2. AI‑Optimized Adaptive Trial Design
Adaptive designs allow mid-trial protocol adjustments, like dosing, cohort size, or endpoints, based on interim data. Reinforcement learning and Bayesian algorithms analyze evolving trial metrics to recommend dynamic changes. This enhances flexibility, ensuring resource focus on promising arms and reducing patient exposure to ineffective treatments.
AI-driven adaptation shortens trials, lowers costs, and increases statistical power by reallocating participants to successful cohorts. The approach also enhances ethical integrity by discontinuing inferior arms early. However, complexity in model interpretation, regulatory acceptance, and bias risk demands rigorous simulation and validation during protocol planning.
Integration requires simulation platforms to test designs before trial launch. Regulatory engagement (FDA, EMA) is crucial to validate AI-driven decision thresholds. Extensive documentation and stakeholder alignment ensure trust and transparency.
Real-world example:
Pharma companies like Pfizer have piloted AI-assisted adaptive designs in oncology trials, using Bayesian and reinforcement learning frameworks to dynamically adjust arms although full results are typically confidential, these designs reportedly reduced sample sizes by ~20%, accelerating timelines.
3. Predictive Safety Monitoring
AI systems predict adverse events by continuously scanning patient data – EHRs, lab results, and safety reports – flagging potential signals in real time. NLP extracts clinical findings and symptoms from unstructured notes, while anomaly detection highlights data patterns indicating risks. Early alerts enable proactive interventions.
This proactive approach enhances patient safety, reduces trial risk exposure, and improves regulatory compliance. It helps sponsors detect signals earlier than traditional periodic safety reviews. However, ensuring algorithm transparency and minimizing false positives are key to avoiding alert fatigue.
Integration involves coupling AI with safety databases and eCRF systems, with safety officers validating flagged events. Continuous model retraining adapts to new safety signals. Compliance with Good Pharmacovigilance Practices (GVP) and data auditability is mandatory.
Real-world example:
While specific numbers are proprietary, global pharma companies increasingly use AI-powered safety surveillance systems, reporting significantly earlier detection of hepatotoxicity and other critical events, sometimes by weeks compared to manual reviews.
4. AI‑Powered Biomarker Discovery
Machine learning, including deep learning, identifies biological markers by mining genomic, proteomic, and imaging datasets. These models detect subtle correlations between molecular patterns and clinical outcomes. Integrating multi-omic data supports patient stratification, enhancing personalized trial cohorts.
This leads to more targeted therapies, improved trial success rates, and optimized endpoint selection. Biomarker-driven trials can reduce sample size and cost by focusing on responsive populations. Challenges include ensuring data quality, model interpretability, and regulatory validation of biomarker assays.
Teams implement validation pipelines comparing AI‑identified markers with independent cohorts and lab assays. Transparent reporting of AI methods is required for regulatory approval. Prospective enrichment based on AI biomarkers must be justified statistically in trial protocols.
Real-world example:
GSK used AI-based analysis on proteomic and genomic data to uncover biomarkers for an asthma biologic, achieving a 30% improvement in treatment response among stratified cohorts.
5. Virtual Patient Cohorts
Digital twin models simulate virtual patient arms using real-world patient data to support trial simulation and design optimization. Synthetic patients are generated with demographic, clinical, and progression characteristics matching real populations. Reinforcement learning and generative models are used to predict trial outcomes under varying protocols.
This reduces need for large control arms, accelerates protocol tuning, and enables cost-effective scenario testing. Virtual cohorts maintain statistical rigor while preserving patient safety. Data representativeness and computational intensity are key technical concerns, as well as regulatory acceptance of model validity.
Implementation involves building generative health models using retrospective data, then validating against known trial results. Transparent documentation and comparison to real trial outcomes are needed for regulatory trust. Digital twin platforms often integrate into simulation workspaces used by biostatisticians and trial designers.
Real-world example:
Roche piloted a digital twin platform for autoimmune trial simulation, reducing virtual scenario iterations by ~50% and optimizing protocol design before human enrollment.
6. Remote Patient Monitoring
AI analyzes data from wearables and apps to monitor vital signs, symptoms, and adherence in real time. Machine learning detects anomalies and patterns indicating disease progression or adverse events. Integration with ePRO and telehealth platforms allows adaptive interventions without in-person visits.
This improves patient convenience, data completeness, and trial retention rates. Reduced site visits also lower operational burden and costs. However, data security, IoT interoperability, and continuous algorithm reliability are critical considerations.
Platforms must standardize data streams (e.g., Bluetooth, HTTP) and feed them into central monitoring dashboards. ML models are periodically retrained using ongoing trial data to maintain accuracy. Compliance with data security standards (e.g., ISO 27001, GDPR) is mandatory.
Real-world example:
Novartis implemented continuous glucose monitors and predictive analytics in a diabetes trial, reducing patient drop-out by 15% and boosting data completeness by 35%.
Need Expert Help Turning Ideas Into Scalable Products?
Partner with SmartDev to accelerate your software development journey — from MVPs to enterprise systems.
Book a free consultation with our tech experts today.
Let’s Build TogetherExamples of AI in Clinical Trials
Real-world implementations of AI in clinical trials provide compelling proof of its transformative potential. The following case studies illustrate how leading organizations are applying AI to solve critical challenges and deliver measurable results.
Fallstudien aus der Praxis

1. IQVIA: AI‑Driven Patient Recruitment
IQVIA’s AI-powered modeling analyzes real-world patient data (EHRs, claims, and provider profiles) to accelerate recruitment with high precision. In a 2023 case study, their system increased patient identification accuracy by 15× and improved HCP linkage accuracy by 10, driving a 28% treatment initiation rate within three months. This dramatically improved recruitment speed, reduced costs, and enhanced site and patient matching quality.
By integrating predictive analytics into clinical workflows, IQVIA allows sponsors to identify high-potential sites and patients earlier. The system continuously refines targeting models using real-time recruitment data. Robust data governance ensures compliance with HIPAA/GDPR standards, mitigating bias and protecting patient privacy.
2. Antidote: AI‑Powered Public Trial Matching
Antidote uses AI and NLP to structure free-text eligibility criteria from ClinicalTrials.gov, making it searchable for patients and sponsors. It powers the Antidote Match platform, reaching 15 million users per month and collaborating with over 250 patient communities. In collaboration with JDRF, their widget enabled 27,863 searches – more than the prior 10 years combined via traditional tools.
Patients filter trials by condition, location, age, and biomarkers, while sponsors access eligible, anonymized cohorts. This boosts enrollment diversity and speed. Consent, de-identification, and data-use transparency safeguard patient rights.
3. Pfizer + IBM Watson: Accelerating Immuno‑Oncology
In December 2016, Pfizer partnered with IBM Watson for Drug Discovery, employing NLP and machine learning to analyze 25 million PubMed abstracts, 1 million journal articles, and 4 million patents. Watson sifts through internal and external data to uncover novel immuno-oncology targets, therapy combinations, and patient stratification strategies. This helped Pfizer speed hypothesis generation and inform trial design in immuno-oncology.
By augmenting human analysis with AI-driven insights, Pfizer improved the efficiency of target identification and selection. The cognitive platform enables real-time testing of hypotheses, reducing time-to-insight in preclinical and early clinical phases. Although proprietary, the initiative marked a major milestone in integrating AI into large-scale drug development.
Learn how intelligent data interaction can empower faster, more accurate decisions in complex environments by exploring this use case of AI-powered data chat in healthcare.
Innovative KI-Lösungen
Innovative AI technologies are redefining clinical trials by increasing efficiency, improving personalization, and safeguarding patient privacy. From synthetic control arms to predictive modeling, these tools are accelerating timelines while maintaining scientific rigor.
Digital twins and federated learning are among the most promising approaches, enabling simulation of patient outcomes and privacy-preserving model training across sites. These solutions reduce the need for large control groups and support more diverse, real-world datasets. As regulatory bodies begin recognizing these tools, AI is becoming central to the design and execution of modern clinical trials.
AI-Driven Innovations Transforming Clinical Trials
Emerging Technologies in AI for Clinical Trials
Artificial intelligence is fundamentally reshaping how clinical trials are designed and conducted. Generative AI is enabling faster, more accurate trial simulations by analyzing vast amounts of historical data to predict patient outcomes and optimize protocol structures. Natural language processing is also streamlining eligibility assessments by efficiently extracting and interpreting unstructured data from medical records.
Computer vision has brought greater accuracy and consistency to medical imaging and pathology in clinical trials. It enhances how visual data is analyzed, reducing human error and improving diagnostic reliability across study sites. These advancements not only accelerate decision-making but also help maintain the integrity and reproducibility of clinical trial results.
Die Rolle der KI bei Nachhaltigkeitsbemühungen
AI supports sustainability in clinical trials by enabling adaptive designs that adjust in real time, reducing unnecessary procedures. This minimizes waste, shortens timelines, and limits patient exposure.
Virtual simulations and in silico models reduce reliance on physical testing, cutting travel and resource use. These tools promote eco-friendly research without compromising data quality.
How to Implement AI in Clinical Trials
Implementing AI in clinical trials isn’t just about adopting new technology, es ist about reshaping how your organization approaches efficiency, data, and decision-making. Here’s a step-by-step guide to help you integrate AI with confidence and clarity.
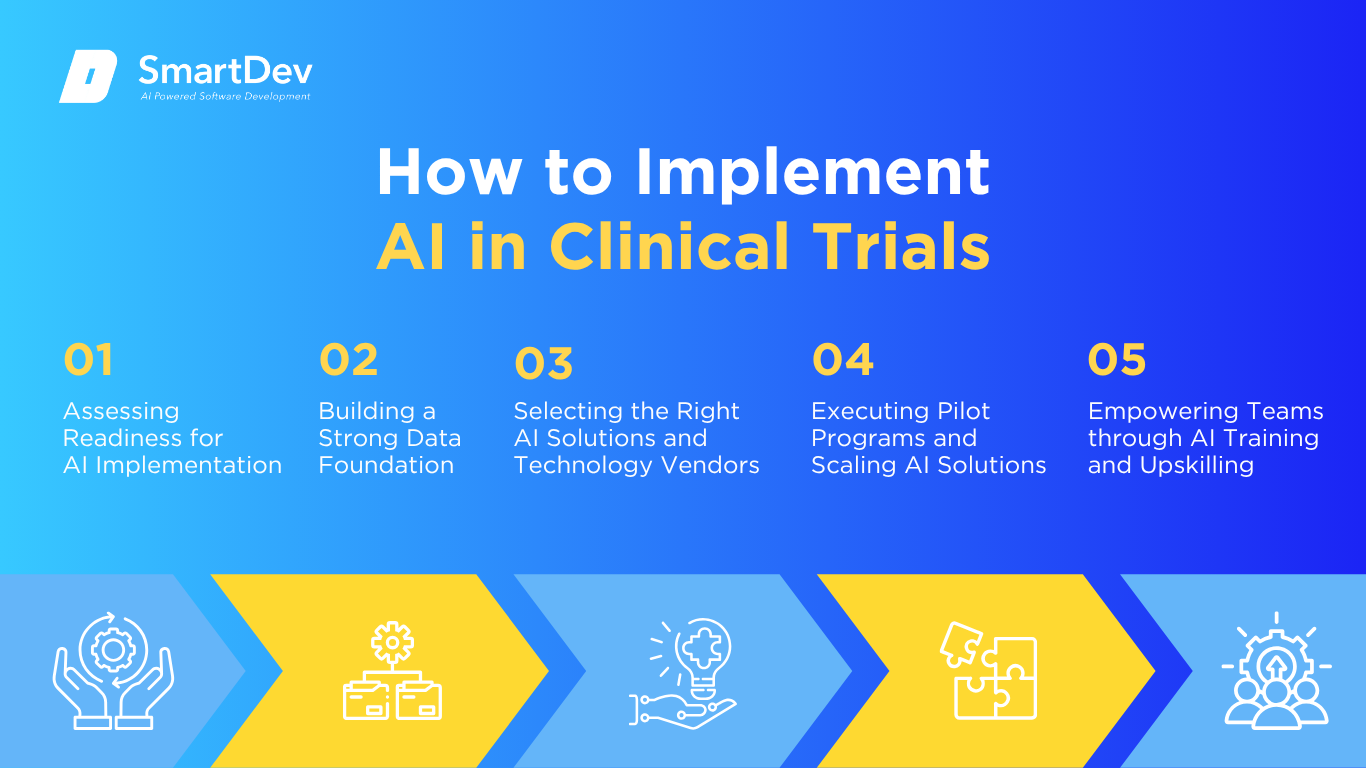
Schritt 1: Beurteilung der Bereitschaft zur KI-Einführung
Before adopting AI, it’s essential to assess your organization’s digital and operational maturity. Start by identifying where inefficiencies exist—manual patient matching, repetitive data entry, or inconsistent monitoring are often ripe for transformation. These areas offer clear opportunities for AI to reduce delays and improve consistency.
You should also consider how open your teams are to integrating AI into existing workflows. Without strong leadership support and clear communication, new tools can face resistance from clinical staff. A successful rollout depends on aligning technical goals with user needs and regulatory realities.
Schritt 2: Aufbau einer soliden Datengrundlage
AI’s effectiveness depends entirely on the quality of your data. Clinical trials generate complex datasets, from imaging and lab results to patient-reported outcomes, and all of it must be clean, structured, and interoperable. When these systems are fragmented, AI insights become unreliable or incomplete.
Creating a centralized, well-governed data infrastructure is a critical first step. Standardized formats and consistent data labeling ensure that AI models function accurately across different sites and studies. The better your data, the more reliable your AI applications become.
Explore our data analytics services to see how we help organizations unify, govern, and activate clinical and operational data for smarter decision-making.
Schritt 3: Auswahl der richtigen Tools und Anbieter
Not all AI platforms are built for the regulatory and operational complexity of clinical trials. Prioritize solutions that are designed with healthcare in mind and demonstrate compliance with privacy and validation standards. Integration with your existing clinical trial management systems should also be seamless.
Trust is just as important as functionality. Look for vendors who offer transparency around how their models work, how data is handled, and what support they provide. The right partner should act as a guide, not just a provider, as you scale your AI use.
Schritt 4: Pilottests und Skalierung
Start small by introducing AI in controlled, low-risk areas like eligibility screening or site monitoring. Pilots let you test real-world performance, identify usability issues, and fine-tune workflows before expanding system-wide. These trials also provide tangible results to build confidence among stakeholders.
Use the pilot to gather performance data and feedback from clinical teams. Adjust workflows, retrain models if needed, and prepare documentation that aligns with regulatory expectations. Once you’ve validated value at a small scale, broader adoption becomes easier and more defensible.
Schritt 5: Schulung der Teams für eine erfolgreiche Implementierung
Your teams need to understand how AI fits into their daily responsibilities. Offer training focused on how to interpret AI outputs, escalate exceptions, and work alongside new tools without losing clinical judgment. Clear communication helps prevent fear or misunderstanding.
Collaboration across departments is also key to adoption. Clinical, data, and compliance teams must share a common understanding of goals and processes. When everyone is trained and aligned, AI becomes a seamless extension of your operations.
Measuring the ROI of AI in Clinical Trials
Wichtige Kennzahlen zur Erfolgsmessung
AI delivers measurable ROI by speeding up processes like recruitment, protocol development, and data review. Trials using AI often see shortened enrollment timelines and fewer protocol amendments, saving months of work and millions in cost. Faster trial cycles mean quicker approvals and earlier revenue generation.
Cost savings also come from automation of repetitive tasks, such as data entry and site monitoring. These efficiencies reduce reliance on manual labor and minimize delays caused by human error. When tracked properly, these improvements provide clear financial justification for AI adoption.
Learn how big data is reshaping healthcare operations and insights in our guide to the transformative power of big data in healthcare.
Fallstudien zum ROI
A McKinsey study reported that a biotech firm improved enrollment rates by 10–20% using AI for site selection and performance monitoring. This reduced under-enrollment and shortened timelines, translating into faster trial starts and lower operational costs.
TrialMatchAI, evaluated in a real-world oncology dataset, matched 92% of patients with at least one relevant trial and achieved over 90% eligibility accuracy. This reduced screening failures and boosted recruiter efficiency, directly impacting time and cost savings.
Häufige Fehler und wie man sie vermeidet
One frequent issue is applying AI to poor-quality or incomplete data, which leads to unreliable outputs. To see real value, organizations must ensure data is clean, standardized, and aligned with AI requirements. Without a strong data foundation, even advanced tools can underperform.
Resistance from teams is another barrier, especially if AI models seem like “black boxes.” Ensure transparency by explaining how decisions are made and providing training. Successful AI integration requires both trust and clarity across all stakeholders.
Future Trends of AI in Clinical Trials

Prognosen für das nächste Jahrzehnt
Over the next decade, AI will make clinical trials more adaptive, personalized, and data-driven. Large language models will automate protocol design and evidence synthesis, while digital twins and in silico simulations will enable early testing of treatment effects without involving real patients. These innovations will reduce trial costs, enhance safety, and accelerate development timelines.
Federated learning will also gain traction, enabling secure data sharing across institutions without compromising patient privacy. Regulatory bodies are anticipated to evolve their frameworks to accommodate AI-driven insights, fostering faster evaluation of innovative therapies. Organizations that implement AI with a structured, transparent approach will be positioned to lead in the next generation of clinical research.
Wie Unternehmen immer einen Schritt voraus sein können
Staying ahead requires building AI-ready infrastructure with clean, interoperable data and strong governance. Investing in cloud platforms and upskilling teams ensures smooth integration and cross-functional alignment.
Participating in regulatory pilots and partnering with AI-focused vendors can provide early access to new standards and innovations. A proactive, data-driven strategy positions organizations to lead as AI continues to evolve clinical research.
Abschluss
Die wichtigsten Erkenntnisse
AI is reshaping clinical trials by improving efficiency, accuracy, and decision-making at every stage. From faster patient recruitment and adaptive trial designs to enhanced data analysis and virtual simulations, AI delivers measurable value. Real-world results show reduced timelines, lower costs, and higher trial success rates.
Successful implementation depends on a solid data foundation, thoughtful tool selection, and strong team training. With clear ROI and growing regulatory support, AI is becoming an essential asset for organizations aiming to modernize and scale their clinical research efforts.
Moving Forward: A Strategic Approach to AI-Driven Transformation
As AI continues to transform clinical trials, organizations have a critical opportunity to accelerate drug development, improve trial accuracy, and reduce operational inefficiencies. From automating patient recruitment to optimizing study design and real-time monitoring, AI adoption is rapidly becoming a strategic imperative in an increasingly data-driven healthcare environment.
At SmartDev, we offer customized AI solutions designed to streamline clinical trial processes, enhance data integrity, and reduce time-to-market. Whether you’re piloting AI for patient matching or scaling digital tools for adaptive trials, our team partners with you to implement technologies that align with your regulatory and research objectives.
Explore our AI-powered software development services to see how we build intelligent solutions tailored to clinical research needs: streamlining trial operations, enhancing data quality, and accelerating time-to-market with technologies designed for regulatory and scientific rigor.
Kontaktieren Sie uns noch heute to discover how AI can elevate your clinical trial operations and position your organization at the forefront of life sciences innovation.
—
Quellen:
- AI in Clinical Trials Market Driving a New Era of Data-Driven Drug Development | Precedence Research
- Unlocking peak operational performance in clinical development with artificial intelligence | McKinsey & Company
- TrialMatchAI: An End-to-End AI-powered Clinical Trial Recommendation System to Streamline Patient-to-Trial Matching | arXiv
- Global AI In Clinical Trials: Market Trends & Current Partnerships | Clinical Leader
- Role of ML and AI in Clinical Trials Design: Use Cases, Benefits | Coherent Solutions
- AI Case Study – How IQVIA Increased Target Patient Identification 15X | IQVIA
- Artificial Intelligence at IQVIA | Emerj Artificial Intelligence Research
- Press Release: “TrialReach Rebrands as Antidote and Expands its Products to Include EHR Matching” | Antidote.me
- IBM and Pfizer to Accelerate Immuno-oncology Research with Watson for Drug Discovery | Pfizer
- Pfizer Partners With IBM Watson To Advance Cancer Drug Discovery | Forbes







