Introduction
Healthcare is at a breaking point. Rising patient loads, clinician burnout, and growing cost pressures are straining systems worldwide. AI in health is no longer just a buzzword; it’s a practical solution reshaping clinical care, diagnostics, operations, and patient engagement. This comprehensive guide explores how AI is redefining healthcare delivery, boosting efficiency, and opening new frontiers in medical innovation.
What is AI and Why Does It Matter in Health?
Definition of AI and Its Core Technologies
Artificial Intelligence (AI) refers to systems that perform cognitive functions such as learning, reasoning, decision-making, and pattern recognition. Key technologies include machine learning for pattern-based predictions, natural language processing (NLP) for analyzing clinical documentation, computer vision for medical imaging, and generative AI for clinical summarization and automation.
In health, AI enables faster diagnostics, predictive risk scoring, workflow automation, and personalized care at scale. From analyzing radiology scans in seconds to drafting discharge summaries and powering virtual health assistants, AI is directly addressing healthcare’s most pressing challenges: clinician burnout, operational inefficiencies, and patient access barriers.
The Growing Role of AI in Transforming Health
AI is fundamentally transforming how care is delivered, documented, and scaled. In diagnostics, tools like Aidoc and Viz.ai use computer vision and machine learning to detect strokes, fractures, and cancer with sub-minute precision, supporting radiologists and improving emergency response times. AI now flags life-threatening conditions from routine scans, enabling earlier intervention and improved survival rates.
Clinical workflows are also being redefined. Generative AI is powering ambient scribing tools that automatically capture and structure patient-doctor conversations, reducing documentation time by over 50%. At the same time, large health systems like HCA Healthcare are piloting AI agents that orchestrate tasks across documentation, billing, and clinical decision support.
Patient-facing applications are gaining traction too. AI chatbots and virtual agents are handling triage, answering medical queries, and providing 24/7 access to reliable guidance—especially valuable in rural or resource-limited settings. These tools expand access while freeing up staff for higher-value clinical interactions.
Key Statistics and Trends in AI Adoption in Health
AI adoption in healthcare is rapidly expanding. The 2024 Medscape & HIMSS AI Adoption in Healthcare Report reveals that 86% of healthcare providers in North America are utilizing AI tools, with applications spanning medical imaging, diagnostics, and administrative automation, such as streamlining clinical workflows and reducing documentation burdens.
Physician engagement with AI is also on the rise. According to a 2025 TempDev report, 66% of clinicians were actively using AI tools in 2024, a significant increase from 38% in 2023. Key use cases include clinical documentation, diagnostic decision support, and delivering personalized care recommendations, enhancing efficiency and patient outcomes.
Market projections reflect this momentum. AIPRM reports the global AI in healthcare market is expected to grow from $32.3 billion in 2024 to $208.2 billion by 2030, at a CAGR of 36.4%. Forward-thinking organizations are integrating AI into core workflows to enhance competitiveness and prepare for future healthcare demands.
Business Benefits of AI in Health
AI delivers measurable value across the healthcare sector by addressing persistent inefficiencies: delayed diagnostics, administrative overload, rising operational costs, and limited access to care. Below are five core business benefits of implementing AI across clinical, operational, and patient-facing workflows:
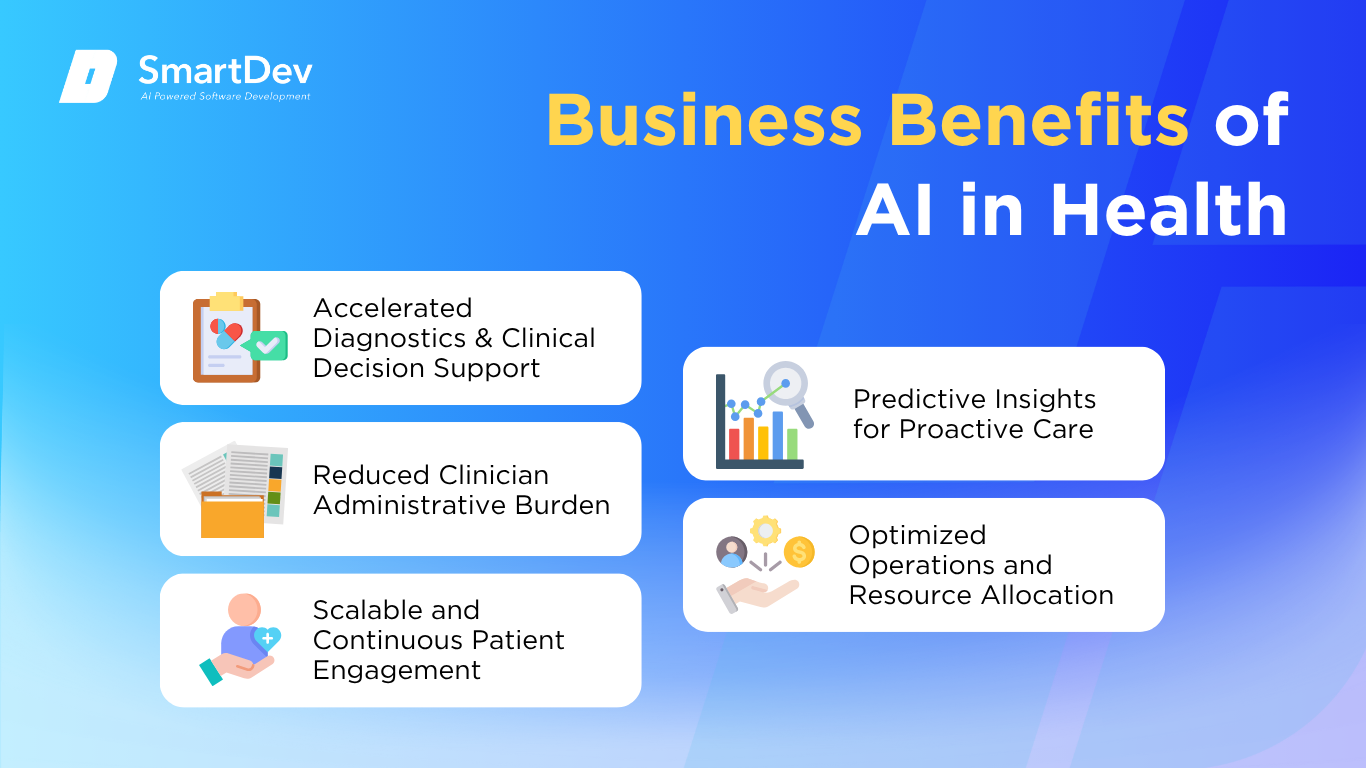
1. Accelerated Diagnostics and Clinical Decision Support
AI enhances diagnostic speed and accuracy by analyzing medical images like CTs and MRIsfaster than traditional reviews. Tools like Aidoc can identify brain bleeds or pulmonary embolisms within minutes, enabling timely interventions during critical care situations. This improves patient survival rates, reduces diagnostic errors, and shortens time-to-treatment.
Beyond imaging, AI-based decision support systems use clinical history and vitals to recommend next steps. At Mayo Clinic, AI models detect early signs of sepsis hours before clinical teams typically would. These predictive capabilities help prevent complications, lower ICU admissions, and support safer, more proactive care.
2. Reduced Clinician Administrative Burden
Natural language processing (NLP) systems like Nuance DAX automatically transcribe physician-patient conversations into structured clinical notes. These tools reduce after-hours charting by up to 80%, allowing providers to focus on patient care instead of paperwork. The result is higher physician satisfaction, reduced burnout, and more engaged interactions with patients.
AI also automates medical coding, order entry, and documentation reviews across EMRs. By streamlining these tasks, it lowers the risk of administrative errors and increases productivity across care teams. Hospitals using AI workflows often report shorter patient throughput times and smoother coordination across departments.
3. Scalable and Continuous Patient Engagement
AI-powered chatbots and virtual agents enable 24/7 patient interaction, handling appointment scheduling, symptom triage, and follow-up reminders. Platforms like Ada and Babylon provide multilingual support, ensuring patients across demographics get accessible and timely assistance. This is particularly valuable in rural or resource-limited areas with limited clinician availability.
Automated engagement improves patient adherence and lowers no-show rates. AI systems can tailor follow-ups based on a patient’s condition, behavior, and treatment plan—personalizing outreach at scale. Healthcare systems benefit by reducing readmissions and freeing clinical staff from routine inquiries.
4. Predictive Insights for Proactive Care
AI models forecast disease progression and acute deterioration by analyzing EHR data, wearables, and genetic markers. Hospitals like Mount Sinai use these models to flag at-risk patients, enabling preemptive interventions before conditions worsen. This reduces preventable hospitalizations and improves care outcomes in chronic and acute cases.
In oncology, AI identifies effective therapies by matching tumor genetics with treatment databases. These precision medicine approaches help personalize care plans, lower treatment failure rates, and reduce side effects. Over time, predictive insights can reshape care delivery from reactive to preventative.
5. Optimized Operations and Resource Allocation
AI supports operational planning by predicting patient admissions, optimizing shift schedules, and managing bed availability. Tools like Qventus allow hospitals to streamline discharges and reduce ER bottlenecks, improving flow and patient satisfaction. These gains are particularly impactful during surges or staffing shortages.
Beyond clinical operations, AI enhances supply chain and billing processes. Machine learning detects claim anomalies, flags potential fraud, and improves revenue cycle accuracy. Financial performance improves as organizations reduce waste, speed up reimbursements, and maintain compliance more effectively.
Challenges Facing AI Adoption in Health
Despite its potential, AI adoption in healthcare faces critical obstacles that can hinder effectiveness and scalability. These challenges are not just technical; they also involve data quality, trust, regulation, and equity.
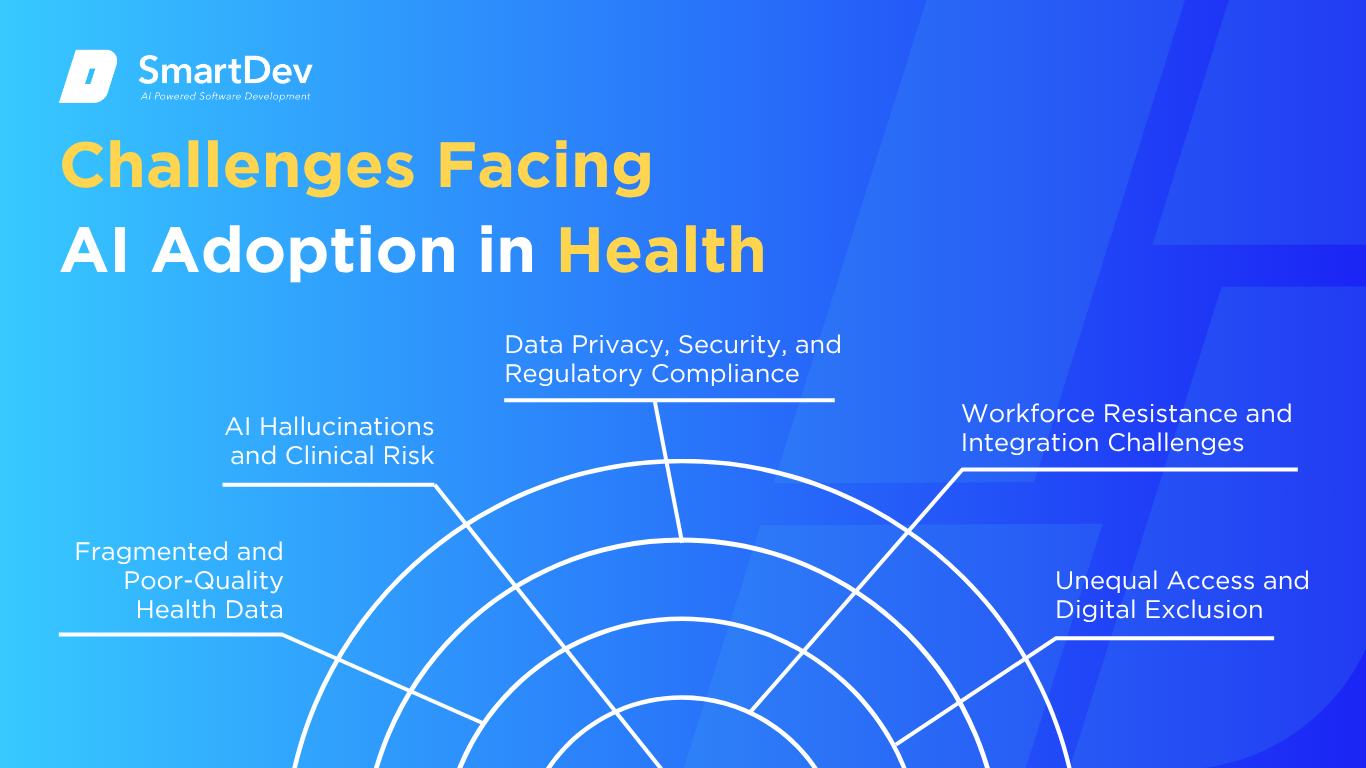
1. Fragmented and Poor-Quality Health Data
AI models depend on large volumes of clean, consistent data, but healthcare data is often fragmented across EHR systems, labs, and third-party providers. Inconsistent coding, missing entries, and incompatible formats reduce the accuracy of AI predictions and limit automation. Without unified, high-integrity datasets, AI cannot generate reliable clinical insights.
Fixing this requires more than just data engineering; it demands data governance, collaboration across departments, and ongoing data validation processes. Organizations must invest in integrating systems and standardizing data flows to enable AI at scale. Until then, AI solutions risk being underutilized or producing misleading outputs.
2. AI Hallucinations and Clinical Risk
Generative AI can produce clinically incorrect or fabricated information, sometimes presented with unwarranted confidence. A recent example involved a Google Med-PaLM model that referenced a non-existent brain structure, raising serious safety concerns. In clinical settings, even small hallucinations can lead to inappropriate care or legal liability.
This makes human oversight essential. Every AI-generated output, especially those involving diagnosis or treatment must be reviewed by licensed professionals. Building guardrails such as confidence scores, red flag alerts, and transparent model documentation is critical to minimize harm.
3. Data Privacy, Security, and Regulatory Compliance
AI systems must comply with strict regulations like HIPAA (in the U.S.) or GDPR (in the EU), which govern how patient data is used and shared. But AI models often require data pooling, third-party processing, or cloud deployment, all of which raise compliance risks. Unauthorized access, data leaks, or insufficient encryption can erode patient trust and expose providers to penalties.
Ensuring compliance requires robust data governance frameworks, vendor accountability, and ongoing audits. Health organizations must also educate staff on proper data handling and AI use policies. Without proactive oversight, privacy concerns may derail AI initiatives even before they scale.
4. Workforce Resistance and Integration Challenges
Clinicians often resist AI tools they perceive as intrusive, opaque, or misaligned with existing workflows. Some fear job displacement, while others distrust “black box” systems that make decisions without clear reasoning. If AI disrupts rather than complements clinician routines, adoption can stall.
Successful integration requires co-designing AI tools with clinical staff, offering transparency, and aligning outputs with familiar decision processes. Training and change management are just as important as technical deployment. Building clinician trust takes time, but it’s vital for sustainable adoption.
5. Unequal Access and Digital Exclusion
While AI tools promise to expand care, they can also worsen disparities if not deployed equitably. Patients without internet access, digital literacy, or modern devices may be excluded from virtual care, remote monitoring, or AI-guided triage. This creates a risk of deepening health inequities across income, geography, and age groups.
To close this gap, health systems must pair AI with human support, accessible interfaces, and inclusive design. Policymakers and providers need to ensure infrastructure and funding reach underserved populations. Equity must be built into AI deployment from day one, not retrofitted after rollout.
Specific Applications of AI in Health
1. AI‑Powered Diagnostic Imaging
AI‑powered diagnostic imaging addresses the challenge of detecting anomalies in medical scans with greater speed and accuracy. Deep convolutional neural networks (CNNs) analyze X‑rays, CT scans, MRI and ultrasound images to identify tumors, fractures, or other conditions that might be missed by human eyes. These systems can rapidly prioritize critical cases and reduce diagnostic delays.
They are trained on vast datasets of labeled medical images and deploy techniques like CNNs and attention mechanisms to highlight suspicious regions. Integration into radiology workflows allows seamless review by radiologists, with AI suggestions annotated directly on the scan viewer interface. This yields faster turnaround times, fewer false negatives, and improved diagnostic consistency across patient populations.
A radiology AI startup deployed its CNN‑based lung nodule detection tool at a hospital network, where it processed thousands of CT scans weekly. They used a combination of in‑house trained networks and the hospital’s imaging archive. After implementation, time to diagnosis reduced by 30% and detection sensitivity improved by 12%.
2. Predictive Analytics for Patient Risk Stratification
Predictive analytics helps healthcare providers identify high‑risk patients proactively, preventing complications and reducing readmissions. Machine learning models analyze structured EHR data (labs, vital signs, demographics) and unstructured notes to forecast risks like sepsis, heart failure, or ICU admission. This enables earlier clinical intervention and personalized care planning.
Models such as gradient boosting machines and recurrent neural networks absorb time‑series and static features to output individual risk scores. Integration into EHR dashboards and clinician workflows enables alerts and risk summaries used in rounds and care coordination. This contributes to proactive care, fewer complications, and cost savings through prevented events.
A major hospital system implemented a gradient boosting model to predict 30‑day readmission risk for congestive heart failure patients. Their analytics team ingested EHR records, lab results, and discharge summaries. Within six months, readmission rates dropped by 15% and average length of stay decreased by one day per patient.
3. Virtual Assistants for Patient Engagement & Triage
Virtual assistants powered by conversational AI enhance patient engagement, providing 24/7 support for symptom checking, scheduling, and medication reminders. These chatbots help health systems reduce administrative burden, improve access, and guide patients to appropriate care settings. They free clinicians to focus on higher‑value tasks and reduce unnecessary emergency visits.
Modern assistants use natural language understanding (NLU) and dialogue management systems trained on medical ontologies and patient conversation logs. They can parse symptom descriptions, ask clarifying questions, and route users to telehealth, in‑person visits, or educational resources. Integration with patient portals and scheduling systems enables seamless user experience.
A healthcare provider launched a chatbot that managed appointment booking, symptom triage, and medication reminders through their mobile app. They used a cloud‑based conversational AI platform integrated with their EHR. The tool reduced call center volume by 35% and increased patient adherence to follow‑up visits by 20%.
4. AI‑Driven Drug Discovery & Development
AI‑driven drug discovery accelerates identification of novel compounds and repurposes existing drugs by analyzing large biochemical datasets and molecular structures. These tools address the high time and cost of traditional R&D, enabling faster candidate selection and optimization. They leverage predictive modeling to prioritize promising leads for in vitro and in vivo testing.
Methods include graph neural networks to model molecular properties, deep generative models for compound synthesis, and reinforcement learning to optimize binding affinity. Integration with high‑throughput screening and lab automation platforms speeds iteration cycles. The result: faster pre‑clinical candidate identification and lower development costs.
A biotech firm used generative AI to design and screen potential antiviral compounds against a novel virus. They combined graph neural networks and neural molecular docking simulations. Within months, they identified a compound with strong efficacy in vitro that entered pre‑clinical testing within six months—cutting typical timelines by over 40%.
5. Personalized Treatment Planning with Genomics‑Driven AI
Personalized treatment planning uses AI to interpret genomic, proteomic, and clinical data to tailor therapies—for example, in oncology where tumor genomics guide treatment choice. This approach addresses the variability in patient response to chemo, targeted therapies, or immunotherapy by predicting likely outcomes. It enhances precision medicine, reducing trial-and-error and improving success rates.
AI methods include ensemble learning and deep neural networks that integrate genomic variants, expression profiles, and clinical history to forecast therapeutic response. These tools interface with clinical decision support systems (CDSS) and tumor board workflows. Providers receive actionable insights such as recommended drug regimens or risk of adverse response.
A precision oncology center adopted an AI platform that analyzed tumor sequencing and clinical data to recommend targeted therapies. They used ensemble neural models trained on thousands of cases. Treatment decisions guided by the system led to a 25% improvement in response rate compared to standard protocols.
6. Operational Efficiency via AI‑Enhanced Scheduling & Workflow Automation
AI‑powered scheduling systems optimize clinical staff rostering, operating room assignments, and patient appointment coordination. Healthcare systems often face inefficiencies due to mismatched staff availability, operating theatre utilization, and patient wait times. AI tools dynamically align resources with demand, improving throughput and reducing costs.
These platforms use reinforcement learning and optimization algorithms fed by historical usage patterns, patient volume forecasts, and staff availability preferences. They integrate with hospital scheduling systems and EHR workflows to automate assignment suggestions, notifications, and contingency plans. The outcome is smoother operations, fewer delays, and better staff allocation.
A hospital chain deployed an AI scheduling system that optimized OR block allocation and staff rosters across multiple sites. Reinforcement learning agents used historical surgical volumes and provider availability. This led to a 20% increase in OR utilization and a 15% reduction in patient wait times.
Need Expert Help Turning Ideas Into Scalable Products?
Partner with SmartDev to accelerate your software development journey — from MVPs to enterprise systems.
Book a free consultation with our tech experts today.
Let’s Build TogetherExamples of AI in Health
AI is becoming a foundational enabler in the healthcare sector, transforming diagnostics, patient care, operations, and pharmaceutical research. Below are three standout examples showcasing how leading organizations are leveraging AI to improve clinical outcomes, streamline workflows, and personalize treatment.
Real-World Case Studies
1. Mayo Clinic: Predictive Analytics for Patient Deterioration
Mayo Clinic has implemented AI‑based predictive analytics to identify hospitalized patients at risk of deterioration. By analyzing EHR data including vitals, lab results, and clinician notes in real time, the system generates early warning scores for potential sepsis, cardiac events, or ICU transfers. These scores trigger alerts to clinicians, allowing proactive intervention.
The system uses machine learning models trained on tens of thousands of historical patient records. Integrated into bedside monitors and nurse dashboards, the tool has led to a measurable drop in mortality and ICU admissions. In trials, Mayo Clinic reported a 17% reduction in rapid response activations and improved clinician response times.
2. Mount Sinai Hospital: AI‑Powered Radiology Workflow Optimization
Mount Sinai Health System uses AI to triage radiology imaging for faster and more accurate diagnosis of urgent conditions. Their AI solution automatically flags chest X‑rays showing signs of pneumothorax, nodules, or pneumonia, pushing these scans to the top of radiologist worklists. This reduces time to diagnosis in emergency cases.
The AI platform, trained on millions of de‑identified images, works seamlessly with PACS and hospital imaging systems. Since deployment, Mount Sinai has reduced radiology turnaround times by 25%, especially in high‑volume emergency departments. This has improved outcomes in critical cases and optimized radiologist workload distribution.
3. Novartis: AI‑Driven Drug Development Acceleration
Novartis is leveraging AI across its R&D pipeline to accelerate target identification, molecule screening, and clinical trial design. Using AI platforms like IBM Watson and in‑house deep learning models, they analyze omics data, trial data, and literature to uncover promising drug candidates and biomarkers. AI tools also help identify patient subpopulations for precision clinical trials.
This AI‑driven approach significantly reduces early‑stage discovery time and trial attrition rates. Novartis reported that AI has enabled a 2‑year reduction in average drug development timelines for select oncology programs. It also helps the company repurpose existing compounds more efficiently by predicting off‑target effects and cross‑indications.
4. Cleveland Clinic: AI‑Enhanced Virtual Assistants for Patient Interaction
Cleveland Clinic deployed AI-powered virtual assistants to improve patient engagement and reduce administrative burdens across its healthcare network. These AI chatbots handle appointment scheduling, symptom checking, pre-visit screening, and post-visit follow-ups via web and mobile platforms. Patients receive quick, consistent support, while staff can focus on higher-priority clinical tasks.
The virtual assistants use natural language processing and are integrated into the clinic’s Epic EHR system to personalize interactions based on patient history. Since implementation, Cleveland Clinic reported a 30% reduction in call center volume and improved patient satisfaction scores in digital interactions. The solution also enhanced access to care by enabling 24/7 support for non-emergency queries.
Innovative AI Solutions
AI-Driven Innovations Transforming Health
Emerging Technologies in AI for Health
Generative AI is redefining how health organizations deliver care, manage data, and support clinicians. These models are being used to automate medical documentation, create personalized patient education, and even simulate disease progression for treatment planning. In hospitals, AI-driven scribes are enabling providers to shift their attention back to patient care by eliminating hours of administrative work.
Computer vision is proving invaluable in diagnostic imaging and real-time health monitoring. Beyond radiology, computer vision powers patient movement tracking in elder care facilities, detects signs of distress in facial expressions, and supports automated screening in remote areas. With cloud integration and real-time analytics, these tools offer faster diagnoses, lower error rates, and scalable access to critical health services, even in underserved regions.
Agentic AI is also emerging as a strategic enabler across health services. By autonomously processing health records, triaging patients, or recommending clinical pathways based on outcomes data, these intelligent agents are supporting complex decision-making without constant human supervision. Whether managing chronic care workflows or guiding public health responses, agentic AI helps systems respond quickly and intelligently, improving both efficiency and patient outcomes.
AI’s Role in Sustainability Efforts
AI is helping health organizations drive sustainability by reducing resource waste, improving preventive care, and optimizing treatment pathways. Predictive analytics models anticipate patient admissions, medication adherence, and disease progression, enabling hospitals to align resources with actual care needs. This leads to fewer unnecessary tests, more efficient staff deployment, and reduced strain on emergency departments.
Energy efficiency is another area where AI is making an impact in health. Smart building systems in hospitals are using AI algorithms to track energy usage, optimize lighting, HVAC, and equipment loads based on occupancy and time-of-day patterns. As sustainability standards in healthcare infrastructure become stricter, AI’s role in monitoring and managing environmental performance will become a vital component of hospital operations.
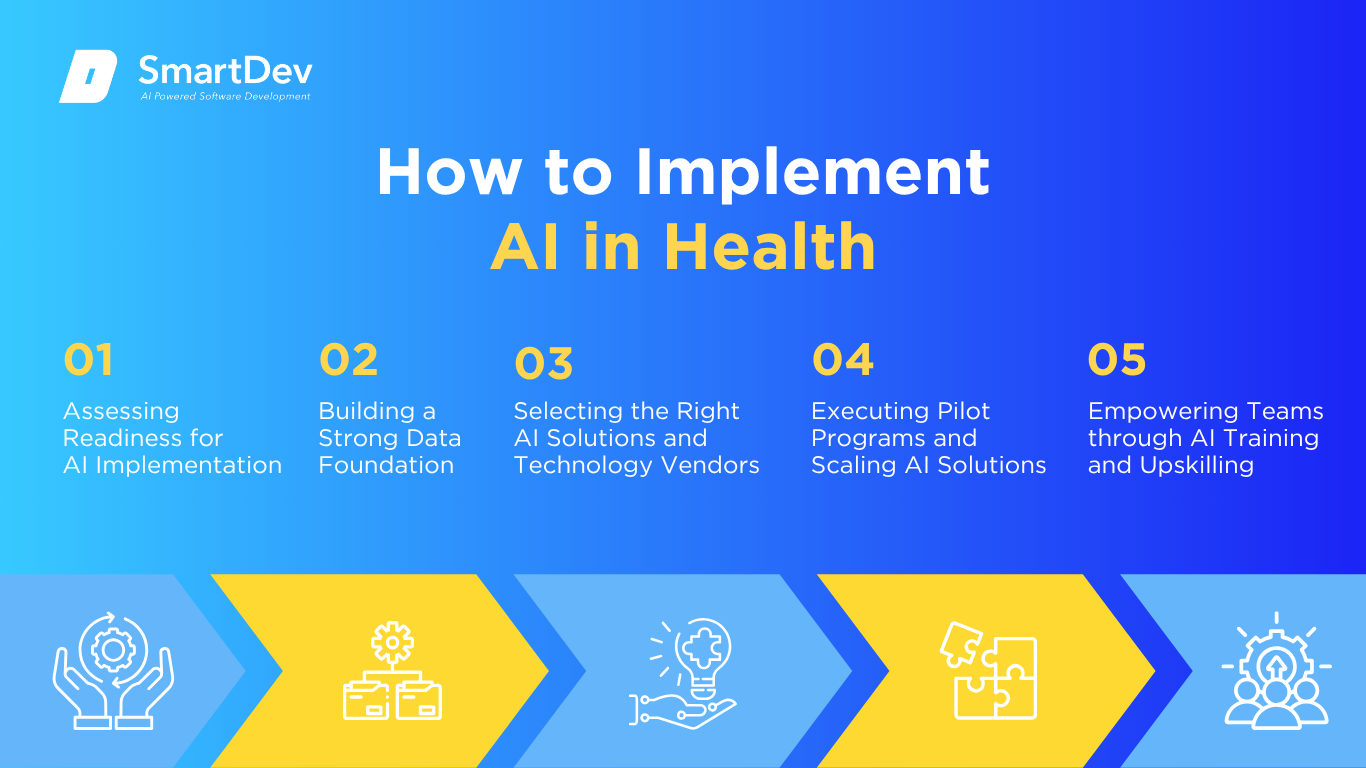
How to Implement AI in Health
Step 1: Assessing Readiness for AI Adoption
Before diving into AI projects, health organizations need to determine where AI can drive the most impact. Common high-value areas include clinical documentation, diagnostic imaging, patient triage, and population health management. These processes often involve high volumes of repetitive tasks and data-heavy decisions, making them ideal use cases for AI integration.
Readiness also includes evaluating your technical infrastructure, leadership alignment, and team capability. Run internal assessments to identify data maturity, system interoperability, and staff openness to digital transformation. Engaging clinicians, IT leaders, and compliance officers early, while setting clear goals to ensure a unified strategy and reduces resistance during implementation.
Step 2: Building a Strong Data Foundation
Clean, structured data is the foundation of any successful AI in health strategy. Start by mapping out where clinical, operational, and behavioral data is collected—EHRs, wearables, imaging systems, and patient portals. Understanding data flow across departments helps identify gaps, redundancies, and opportunities for improvement.
Once you have a clear view, focus on data quality: standardize formats, remove inconsistencies, and ensure secure handling of sensitive information. Compliance with HIPAA, GDPR, or relevant regulations is essential. A well-managed data environment improves AI model accuracy and enables trusted insights that clinicians and administrators can act on.
Step 3: Choosing the Right Tools and Vendors
Choosing the right AI tools in health means balancing regulatory credibility with clinical relevance. Look for platforms that offer FDA-cleared solutions for imaging, scribing, or predictive risk scoring, tools tailored to your organization’s most pressing needs. Integration with your existing health IT systems, including EHRs and PACS, is a must for seamless adoption.
When selecting vendors, prioritize those with proven deployments in health settings and a deep understanding of clinical workflows. The best partners go beyond selling software—they collaborate on implementation, provide training, and offer long-term support to ensure AI evolves with your care delivery model.
Step 4: Pilot Testing and Scaling Up
Jumping straight into full-scale deployment is risky. Instead, start with pilot programs in focused areas, like using an AI scribe in a primary care clinic or computer vision for emergency radiology triage. These pilots help evaluate model performance, gather clinician feedback, and iron out integration issues without overwhelming the system.
Measure success with concrete KPIs: documentation time saved, diagnostic accuracy improvement, patient throughput, or clinician satisfaction. Once results are validated, scale gradually to other departments or sites. A phased rollout approach ensures lessons are learned, feedback loops are maintained, and the tech scales in sync with clinical needs.
Step 5: Training Teams for Successful Implementation
Bringing AI into health requires more than installing software; it demands cultural and operational change. Clinicians, nurses, and administrators need to understand how AI tools work, how to interpret outputs, and when to override or escalate decisions. Upskilling should focus on practical integration into day-to-day workflows.
Equally important is creating a culture of trust around AI. Frame it as a tool to reduce burnout and enhance care, not a replacement for human expertise. Share success stories, involve staff in tool development, and appoint clinical champions who advocate for its use. With the right mindset and training, your teams become empowered AI collaborators—not passive users.
Measuring the ROI of AI in Health
Key Metrics to Track Success
Evaluating the ROI of AI in health requires a balanced look at clinical performance, operational efficiency, and patient outcomes. One of the most immediate indicators is productivity improvement, how much faster doctors can complete documentation, how many more patients radiologists can diagnose, or how effectively care teams can manage chronic conditions. Comparing pre-AI and post-AI metrics in these areas provides tangible insights into gains in throughput and staff utilization.
Cost savings are equally essential to track. AI reduces the manual burden of repetitive tasks like charting, appointment scheduling, or image interpretation. These efficiencies lower overtime costs, minimize administrative overhead, and reduce error-related expenditures. In emergency care, AI-assisted triage tools speed up diagnosis, resulting in shorter hospital stays and fewer unnecessary admissions.
Patient-centric metrics also play a pivotal role in ROI assessment. Early detection tools that improve diagnostic accuracy or predictive models that prevent hospitalizations directly impact quality of care and long-term costs. Improvements in patient satisfaction are increasingly being tied to reimbursement outcomes, further cementing AI’s value.
Case Studies Demonstrating ROI
Stamford Health’s use of AI in detecting heart risk via mammograms illustrates measurable ROI with minimal operational disruption. The AI model, trained on over 20,000 mammograms, identified calcifications tied to future cardiac events. With this insight layered onto routine screenings, the hospital expanded cardiovascular prevention without needing additional scans, lowering long-term treatment costs and improving patient health trajectories.
In the UK, general practices adopting Heidi Health’s AI-powered medical scribe reported dramatic time savings. Over 80% of GPs using the system reduced after-hours documentation and improved patient engagement. This led not only to better clinical efficiency but also to improved work-life balance for staff—a key factor in clinician retention and morale.
Hospitals using Aidoc’s AI for emergency imaging workflows saw improvements in diagnostic speed and accuracy. With stroke and embolism detection occurring within minutes of image upload, treatment times improved significantly. This reduction in diagnostic delay led to faster interventions, lower morbidity rates, and cost reductions from fewer complications and shorter inpatient durations.
Common Pitfalls and How to Avoid Them
A common pitfall in health AI implementation is focusing on innovation without linking it to real clinical challenges. Deploying AI for novelty’s sake often results in clinician frustration and minimal ROI. Each AI initiative should start with a defined problem, measurable goals, and a clear value hypothesis.
Data integrity is another critical challenge. Poorly labeled, incomplete, or siloed health data can lead to misleading model outputs and clinician distrust. Health systems must prioritize data standardization, privacy compliance, and continuous quality monitoring to ensure AI remains reliable and safe.
Lastly, cultural resistance from clinical staff can derail even technically sound projects. Many healthcare professionals remain skeptical of AI due to fears of job displacement or mistrust in algorithmic decisions. To overcome this, leaders must invest in training, foster transparency, and highlight early success stories that position AI as a partner in the care journey.
Future Trends of AI in Health

Predictions for the Next Decade
As AI technology advances, the next decade will redefine how the global health ecosystem delivers care, predicts outcomes, and engages patients. AI in health will shift from augmenting discrete tasks to orchestrating entire care pathways, from preventive screening and early diagnosis to treatment planning and real-time monitoring.
We’ll also see AI converge with wearables, remote sensing, and edge computing, enabling continuous, real-time patient monitoring and intervention outside traditional care settings. LLMs will evolve to be task-specific, domain-trained, and capable of natural dialogue in clinical language, assisting not just with data, but with decisions.
As AI agents become more autonomous and adaptive, they will proactively manage patient care plans, optimize resource allocation in hospitals, and predict public health risks with minimal lag—making precision medicine scalable and more equitable.
How Businesses Can Stay Ahead of the Curve
To stay competitive, health organizations must embed AI into the core of their long-term strategic planning. That means shifting from siloed tech trials to building system-wide AI readiness—aligning leadership, clinical workflows, and data infrastructure around digital-first models. Executives need to champion AI not just as a tech solution, but as a vehicle for operational transformation and value-based care delivery.
Developing in-house AI expertise or forming strategic alliances with tech vendors, research institutions, and regulatory bodies will be critical. Investing in modular, interoperable AI systems, backed by strong data governance and ethical oversight will position organizations to adapt swiftly to innovation.
Cultivating a culture of experimentation, continuous upskilling, and cross-functional collaboration will separate industry leaders from laggards. In the decade ahead, those who treat AI as a strategic co-pilot, rather than a side tool, will be the ones to reshape the future of health.
Conclusion
Key Takeaways
AI is reshaping the health landscape by improving clinical accuracy, reducing operational friction, and enabling more proactive, personalized care. From ambient scribing and imaging diagnostics to chronic disease prediction and energy optimization, AI is no longer a future concept; it’s an essential pillar of modern health strategy.
Organizations that invest in strong data foundations, focus on high-impact applications, and foster AI literacy across teams are seeing measurable returns in both outcomes and efficiency. As AI evolves from assisting with tasks to orchestrating care pathways, its ability to learn, adapt, and personalize will define the next generation of patient experience and system performance.
Health is at a critical crossroads. The choices leaders make today, around integration, governance, and culture, will determine whether they lead or lag in tomorrow’s AI-powered ecosystem.
Moving Forward: A Strategic Approach to AI in Health
If your organization is ready to unlock the full potential of AI in health, now is the time to act with purpose. Begin by identifying where AI can drive the greatest impact, whether it’s accelerating diagnosis, reducing clinician burnout, or expanding access to care. Build a clean, secure data infrastructure, collaborate with proven vendors, and embed a mindset of innovation and continuous learning across your workforce.
At SmartDev, we partner with health systems, clinics, and innovators to build AI strategies that are practical, compliant, and outcomes-driven. From selecting the right technologies and launching successful pilots to training staff and measuring ROI, we guide your AI journey every step of the way. Whether your goal is to elevate patient outcomes, optimize operations, or drive sustainable growth, we’re here to make AI work for you.
The future of health is intelligent. Let’s lead it together!
—
References:
- AI in Healthcare Statistics | AIPRM
- 65 Key AI in Healthcare Statistics | TempDev
- 2024 Medscape–HIMSS AI Report | Medscape
- Cleveland Clinic Announces Rollout of Ambience Healthcare’s AI Platform | Cleveland Clinic Newsroom
- Responsible Use of AI Systems | Novartis
- Mount Sinai First in U.S. to Use AI to Analyze COVID-19 Patients | Mount Sinai
- Artificial Intelligence in Health Care: Benefits, Risks, and Challenges | PMC