Introduction
Healthcare systems worldwide are grappling with rising costs, provider burnout, and escalating demand for personalized patient care. Artificial Intelligence (AI) is stepping in as a game‑changer – streamlining diagnostics, automating workflows, and enhancing treatment personalization. This post explores how AI is reshaping healthcare operations, outcomes, and patient experiences.
Qu'est-ce que l'IA et pourquoi est-ce important dans Healthcare Industry?
Definition of AI and Its Core Technologies
Artificial Intelligence refers to computer systems capable of performing tasks usually requiring human intelligence – learning, reasoning, and decision-making. It spans technologies like machine learning, natural language processing (NLP), computer vision, and generative AI (e.g., large language models) to authoritative sources.
In healthcare, AI leverages these capabilities to aid in diagnostics, personalized medicine, workflow automation, and patient engagement, empowering clinicians and elevating care quality.
The Growing Role of AI in Transforming Healthcare Industry
AI is rapidly transforming clinical and operational processes across the healthcare industry. Hospitals are using AI in diagnostic imaging to detect strokes, tumors, and other critical conditions, while natural language processing (NLP) tools are automating the transcription of clinical notes, saving 40 to 90 minutes of documentation time per provider each day.
Beyond clinical tasks, AI is streamlining administrative functions such as billing and claims processing. In large healthcare organizations, these systems are saving more than 15,000 work-hours per month, allowing staff to reallocate time toward patient care and other high-priority tasks.
At the same time, AI is playing a growing role in expanding healthcare access and responsiveness. Emerging applications are supporting remote patient monitoring, triaging, and real-time decision support, particularly valuable in underserved or resource-limited settings.
Key Statistics and Trends Highlighting AI Adoption in Healthcare Industry
AI adoption in healthcare is rapidly gaining momentum. According to Deloitte’s 2024 report, 80% of hospitals now use AI for workflows or patient care, and 46% are leveraging generative AI tools. Additionally, over 340 FDA-approved AI systems are in diagnostic use, helping detect conditions like stroke, brain tumors, and breast cancer with greater speed and precision.
Healthcare executives strongly support AI integration, with 95% endorsing its adoption and 72% already using generative AI in some capacity. This widespread confidence reflects growing recognition of AI’s role in improving operational efficiency and clinical outcomes.
The return on investment is compelling for early adopters. Organizations report earning $3.20 for every dollar spent on AI, typically realizing these gains within 14 months through cost reductions and faster, more accurate decision-making.
Business Benefits of AI in Healthcare Industry
AI is solving some of the most pressing challenges in healthcare – from administrative inefficiencies to clinical variability – by enhancing accuracy, reducing workload, and enabling more proactive care delivery.
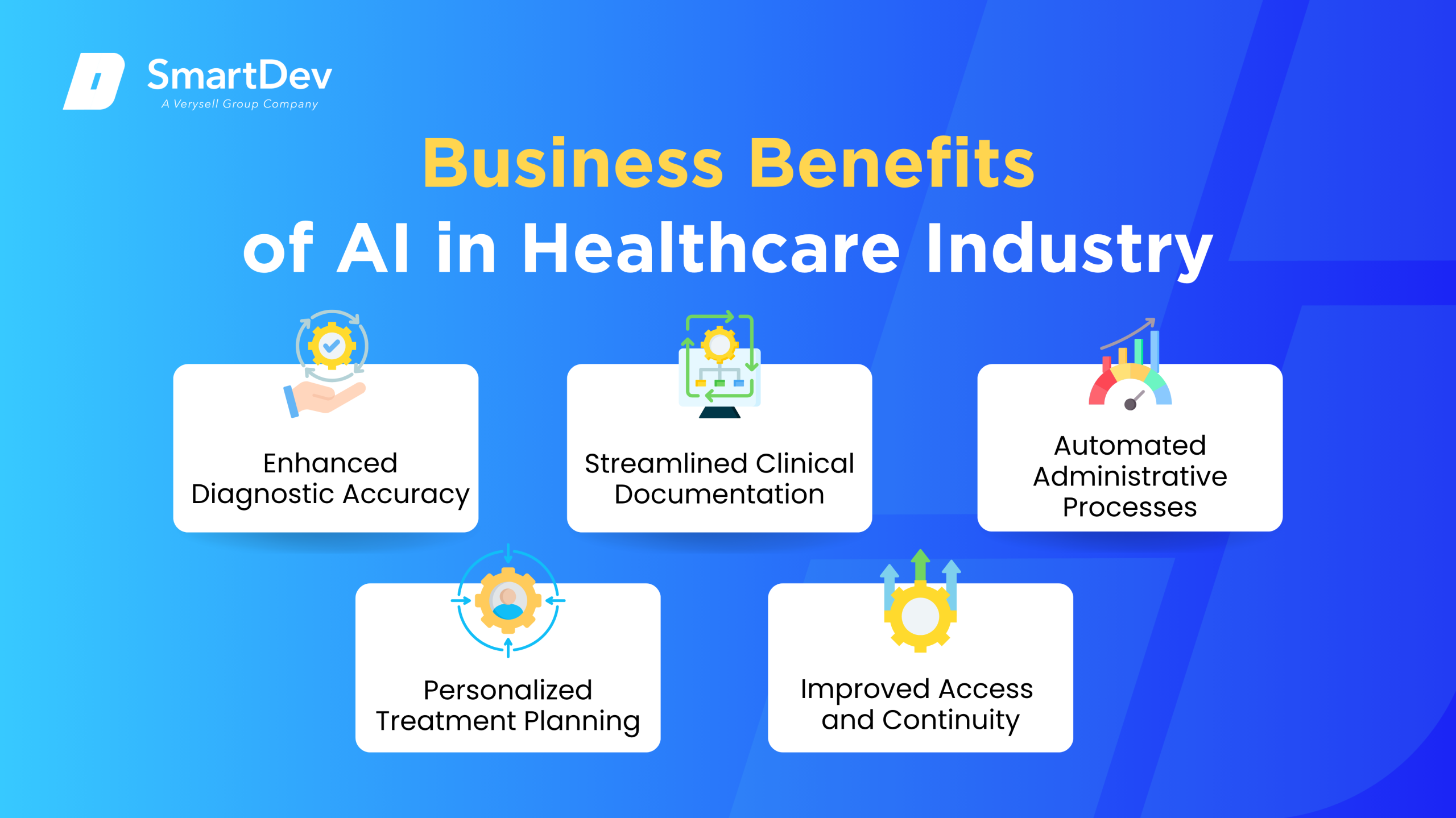
1. Enhanced Diagnostic Accuracy
AI algorithms can analyze large volumes of clinical data, such as imaging or lab results, with a level of consistency and speed that exceeds manual review. This improves diagnostic precision and helps reduce human error in time-sensitive or complex cases.
More accurate diagnostics also support earlier interventions, which can lead to better patient outcomes and reduced treatment costs. The consistency of AI-driven assessments ensures standardized care across different providers and institutions.
2. Streamlined Clinical Documentation
By leveraging natural language processing, AI can automatically transcribe and summarize clinical conversations into structured records. This significantly reduces the documentation burden on healthcare providers, freeing up valuable time.
With less time spent on administrative tasks, clinicians can focus more on direct patient care. This not only improves provider productivity but also enhances the patient experience through more attentive and personalized interactions.
3. Automated Administrative Processes
AI automates routine administrative functions like billing, claims processing, and appointment scheduling. These efficiencies reduce manual workloads and minimize the risk of errors in complex financial or operational workflows.
Operational automation also leads to faster reimbursement cycles and improved cash flow. For healthcare systems under cost pressure, these gains contribute directly to financial sustainability and staff retention.
4. Personalized Treatment Planning
AI can synthesize patient data, ranging from genomics to lifestyle factors, to support highly individualized treatment strategies. This approach enhances the effectiveness of care by tailoring interventions to each patient’s unique profile.
Personalization helps reduce trial-and-error in treatment, potentially lowering the risk of complications or adverse reactions. Over time, this data-driven approach contributes to more consistent and optimized health outcomes.
5. Improved Access and Continuity of Care
AI-powered tools can support care delivery in remote or underserved areas through digital triage, virtual consultations, and remote monitoring. These capabilities help bridge gaps in specialist access and reduce patient wait times.
Continuity of care is strengthened through AI’s ability to track and interpret patient data over time. This allows for proactive interventions and better long-term management of chronic conditions.
To explore how telemedicine is evolving alongside AI, check out our article on transforming the future of telemedicine and healthcare.
Les défis de l'adoption de l'IA dans Healthcare Industry
Despite its potential, AI implementation in healthcare faces several critical barriers. These challenges span data quality, regulation, user trust, and system integration, each requiring thoughtful strategies to overcome.

1. Données fragmentées et de mauvaise qualité
Healthcare data is often stored across disparate systems, from electronic medical records to lab databases, leading to fragmentation and inconsistency. Without clean, well-structured data, AI models struggle to generate reliable or generalizable outputs.
Improving data quality requires more than just technical solutions, it demands organizational alignment around data governance, standardization, and interoperability. Without this foundation, AI’s potential remains largely untapped.
2. Regulatory Complexity and Compliance Risks
AI tools used in clinical care must meet strict regulatory standards, including validation and approval by health authorities. Navigating these processes can delay deployment and limit the speed of innovation.
In addition, compliance with privacy regulations such as HIPAA or GDPR is essential, especially when handling sensitive patient data. Healthcare organizations must implement robust safeguards to manage these legal and ethical responsibilities.
3. Clinician Trust and Ethical Concerns
Many healthcare providers remain cautious about relying on AI due to concerns over transparency and accountability. If clinicians do not understand how AI systems reach conclusions, they may be reluctant to act on their recommendations.
There are also ethical issues, such as algorithmic bias and unequal performance across patient populations. Addressing these concerns requires rigorous testing, explainable AI methods, and inclusive data sets during model development.
4. Workflow Integration and Usability Barriers
AI solutions often face resistance when they disrupt established clinical workflows. If tools are poorly integrated with existing systems or add complexity, adoption rates can suffer significantly.
Effective implementation requires designing AI tools that align with day-to-day clinical practices. Training, change management, and user-centered design are critical to ensuring that AI complements rather than complicates clinical tasks.
5. Cost and Unclear Return on Investment
The upfront investment for AI, including software, infrastructure, and integration, can be a major barrier, especially for smaller organizations. Without clear metrics, stakeholders may struggle to justify the expenditure.
Proving ROI requires defined use cases, measurable outcomes, and long-term commitment to scaling successful pilots. Organizations must adopt a strategic approach to ensure AI delivers sustainable financial and operational benefits.
Specific Applications of AI in Healthcare Industry
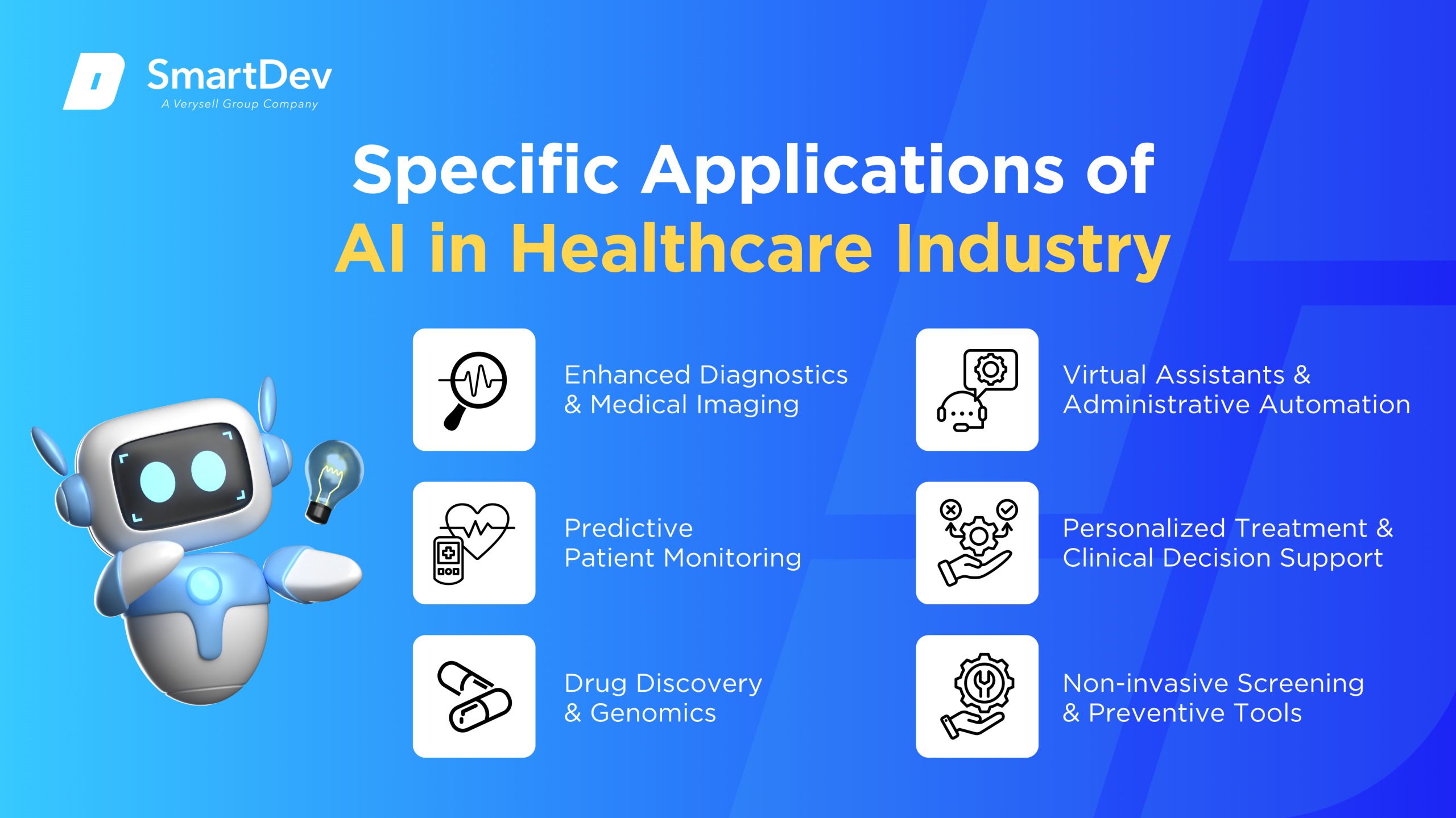
1. Enhanced Diagnostics and Medical Imaging
AI is transforming medical imaging by analyzing scans such as X-rays, CTs, and MRIs to detect anomalies faster and more accurately than traditional methods. These systems are designed to flag critical issues like strokes, hemorrhages, or cancers, helping clinicians prioritize urgent cases. This not only accelerates diagnosis but also reduces the risk of human error in early detection.
The core of this application lies in deep learning models, particularly convolutional neural networks, trained on massive datasets of labeled medical images. These models learn patterns and abnormalities, providing real-time insights directly into radiology workflows. Integration often occurs via PACS systems or cloud platforms that enable seamless use in hospital infrastructure.
The strategic value includes significant improvements in speed, diagnostic precision, and staff productivity. Hospitals benefit from earlier treatment interventions and streamlined triage. However, accuracy depends heavily on data quality and poses challenges in terms of regulatory approval and explainability.
Real-world example:
Aidoc at Mercy Health System: Mercy Health integrated Aidoc’s FDA-approved AI platform to flag urgent pathologies in CT scans. Using deep neural networks, the system accelerated the detection of strokes and pulmonary embolisms. As a result, time-to-diagnosis was significantly reduced, improving emergency care outcomes.
2. Predictive Patient Monitoring
AI-powered patient monitoring systems analyze data from wearable devices to continuously assess patient health in real-time. This is especially useful for managing chronic conditions like heart disease or diabetes, where early detection of deterioration can prevent hospitalization. Algorithms process vitals such as heart rate, blood pressure, and oxygen levels to alert care teams instantly.
The technology utilizes time-series analysis and anomaly detection, powered by machine learning models trained on both population-level and personalized data. Integration with EHR systems ensures that flagged alerts are contextually aware of patient history. Cloud platforms host these analytics, providing scalability and real-time accessibility.
These systems offer strategic advantages such as reduced hospital readmissions, lower emergency response times, and improved patient engagement. Clinicians gain deeper insights into disease progression trends, while patients benefit from proactive rather than reactive care. Ethical issues include data privacy, device reliability, and false alarms, all of which must be managed carefully.
Real-world example:
Cancer RPM Study: A remote monitoring program for cancer patients used wearable sensors and AI to analyze real-time health data. The initiative reduced re-hospitalization rates from 13% to 2.8% and improved patient comfort. It also helped detect post-surgical medication errors 30% more efficiently than manual methods.
3. Drug Discovery & Genomics
AI is streamlining drug discovery by identifying potential compounds, simulating molecular interactions, and predicting clinical efficacy. It addresses the high cost and time requirements of traditional R&D by narrowing down viable candidates faster. Especially in genomics, AI deciphers vast DNA sequences to understand disease links and personalize therapy.
Underlying methods include deep learning, reinforcement learning, and generative models applied to biochemical and genomic datasets. AlphaFold, for instance, revolutionized protein structure prediction using transformer-based AI. These models accelerate preclinical research by predicting how molecules interact with disease targets.
The value is evident in reduced discovery timelines, improved precision in targeting, and revitalization of stagnant pipelines. AI not only shortens time-to-market but enhances the probability of regulatory success. Challenges include validation, ethical use of genetic data, and the reproducibility of AI-driven discoveries.
Real-world example:
Parkinson’s Drug Research: In 2024, AI was employed to screen inhibitors of alpha-synuclein aggregation, a key process in Parkinson’s disease. The use of machine learning reduced screening time by a factor of ten. This enabled researchers to rapidly move from candidate discovery to preclinical testing.
4. Virtual Assistants & Administrative Automation
Administrative burden in healthcare is a major pain point, with clinicians often overwhelmed by documentation and billing tasks. AI virtual assistants and automation tools now handle routine inquiries, appointment scheduling, transcription, and insurance claims. This allows medical professionals to focus more on patient care.
Robotic Process Automation (RPA) combined with Natural Language Processing (NLP) can scan documents, extract structured data, and automate workflows across disparate systems. These tools are deployed on cloud platforms or integrated directly into EHR systems. AI language models also generate clinical notes based on speech inputs, reducing manual typing.
The operational value is immense: reduced administrative costs, faster processing, and fewer errors in patient records and claims. Healthcare providers see measurable gains in staff productivity and service delivery speed. However, privacy compliance, data integrity, and handling edge cases remain areas of concern.
Real-world example:
Omega Healthcare & UiPath: Omega used UiPath’s AI-powered document automation to handle over 250 million healthcare transactions. The solution cut document turnaround time by 50%, saving 15,000 hours per month in manual work. It also improved claims accuracy with a reported 99.5% success rate.
Explore how AI-powered assistants improve user engagement and reduce manual effort in our article on virtual AI assistants.
5. Personalized Treatment & Clinical Decision Support
Personalized treatment uses AI to tailor care plans based on individual genetics, health history, and lifestyle. Clinical Decision Support Systems (CDSS) powered by machine learning provide real-time recommendations to physicians. This enhances treatment efficacy and reduces trial-and-error in prescribing.
These systems analyze EHRs, diagnostic results, and genomics using supervised learning and ensemble methods. They also utilize data fusion from imaging and lab tests to provide context-rich suggestions. Integration into clinical dashboards ensures that recommendations are accessible at the point of care.
Strategically, AI enables precision medicine by minimizing adverse events and boosting treatment alignment with patient profiles. These systems also improve diagnostic confidence and help reduce variability in care standards. However, potential biases in training data and opaque model decisions are key challenges to address.
Real-world example:
Mount Sinai Fair AI Initiative: Mount Sinai deployed an AI framework to audit treatment recommendation systems for demographic bias. Their findings led to updated protocols ensuring equitable care recommendations across patient groups. This initiative highlights the need for fairness in AI-driven clinical decision-making.
Complementing AI-enabled clinical decision tools, intelligent data chat interfaces are driving more informed care – detailed further in our article on AI-powered data chat in healthcare.
6. Non-invasive Screening & Preventive Tools
AI-based non-invasive screening tools are providing fast, accessible triage for diseases such as cardiovascular disorders and skin cancer. Using audio and image data from smartphones or basic sensors, these tools identify high-risk cases. They bring diagnostics to underserved areas with minimal infrastructure.
Machine learning models trained on acoustic biomarkers or dermatological image datasets power these solutions. Cloud processing enables near-instant analysis and decision support through mobile apps. These tools often use transfer learning to maintain high accuracy even with smaller, localized data.
Their advantages include democratizing healthcare access, enabling early detection, and reducing burden on healthcare systems. Clinical validation is essential to ensure reliability and avoid false positives. Privacy, data security, and user training are also crucial for widespread adoption.
Real-world example:
Circadian AI by Siddharth Nandyala: This smartphone-based tool analyzes heart sounds to detect valve disease and heart failure in just seven seconds. It demonstrated 96%+ accuracy in trials with over 18,000 patients. It is now in use across clinics in the U.S. and India, enhancing rural diagnostics.
Examples of AI in Healthcare Industry
AI is no longer just a concept in healthcare, c'est making a real difference in hospitals and clinics around the world. These real-world examples show how organizations are using AI to improve care, speed up processes, and make smarter decisions.
Études de cas réels
1. Mercy Health System & Aidoc – AI-Accelerated Imaging
Mercy Health System partnered with Aidoc to deploy the FDA- and CE-cleared aiOS™ platform across its 50 hospitals and clinics, providing real-time analysis of CT and X-ray images. The AI flags critical conditions like bleeds, pulmonary embolisms, and incidental findings, streamlining radiologist workflows without needing extra infrastructure. This “always-on” solution helps prioritize urgent cases, reducing delays and addressing clinical capacity challenges.
Aidoc’s algorithm is being used enterprise-wide at Mercy as of February 2025 – clinicians report fewer missed urgent findings and smoother implementations. By embedding AI into routine image review, Mercy gains a consistent second check without additional cost to patients. This initiative illustrates how scalable AI tools can help mitigate radiologist shortages and improve care quality systematically.
2. Omega Healthcare & UiPath – Administrative Automation
Omega Healthcare Management Services partnered with UiPath around 2020 to integrate AI-powered Document Understanding into its document workflows, handling billing, claim submissions, and correspondence. This AI augmentation processed over 100 million transactions and freed employees from repetitive tasks, automating 60–70% of client operations. The result was impressive: over 15,000 employee hours saved per month, a 40% reduction in documentation time, a 50% faster turnaround, and 99.5% accuracy for clients.
The use of AI-driven RPA enabled Omega to deliver a strong 30% return on investment to its healthcare clients. Manual review remains integral, but employees shifted focus to exceptions and strategic decisions. This case demonstrates how intelligent automation can cut costs and enhance efficiency in healthcare administration.
3. NHS & Skin Analytics (Derm) – Mobile Skin Cancer Screening
The NHS in the UK deployed Skin Analytics’ AI tool “Derm” across 20 hospitals, enabling staff to perform instant melanoma screening using iPhones and dermatoscope attachments. The AI tool analyzes images in seconds, ruling out benign lesions on the spot so that approximately half of patients avoid specialist referrals. It has flagged over 13,000 cancers and achieved ~99.9% accuracy at excluding melanoma, easing dermatologist workload and reducing wait times.
Clinical data show DERM has a sensitivity of about 97% for malignant melanoma and helps discharge around 40% of urgent referrals early. Hospitals like Chelsea & Westminster saw their average wait time for urgent referrals drop from 14 days to just 3 days. This implementation exemplifies how frontline AI tools can improve triage efficiency and target specialist resources to higher-risk cases.
Solutions d'IA innovantes
Emerging generative AI models, such as large language models, are increasingly being incorporated into radiologist workflows to tackle routine administrative tasks like report drafting and patient communication. In radiology, tools from companies like Bayer and Rad AI are already assisting with transcription-based reporting and follow-up management, which allows clinicians to focus on complex image interpretation. While these systems currently avoid diagnostic decision-making due to regulatory constraints, clinicians forecast broader adoption over the next few years, shifting rather than replacing human roles
Meanwhile, multimodal AI systems, which integrate text, images, lab results, and other data, are transforming care delivery by enabling richer insights across patient records. Models such as PaLM-E-based biomedical platforms and Artera’s prostate cancer treatment system have demonstrated the power of combining diverse data sources for more personalized recommendations. However, significant challenges remain around model explainability, ethical governance, and the need for large-scale clinical validation before wider deployment
To see how AI agents are transforming industries beyond healthcare, check out our insights on AI agent use cases.
AI-Driven Innovations Transforming Healthcare Industry
Healthcare is rapidly embracing artificial intelligence – Gen AI, computer vision, predictive analytics, and automation are reshaping care delivery, diagnostics, and operational efficiency across hospitals and health systems worldwide.
Emerging Technologies in AI for Healthcare Industry
Generative AI is being integrated into clinician workflows, especially in radiology, where tools draft reports and communicate with patients, freeing specialists to focus on complex image interpretation. Aidoc’s aiOS platform, now deployed at Mercy hospitals, enhances imaging speed and diagnostic accuracy. AI-enabled hospital info systems use NLP to automate billing, coding, scheduling, and documentation, thereby reducing clerical workload and cutting operational costs
Computer vision and predictive analytics enhance diagnostics – AI models now detect heart attacks twice as fast with 99.6% accuracy and improve readmission forecasts by over 15%. These systems process vast datasets – EHRs, imaging, labs – to surface insights that empower earlier and more precise interventions.
Le rôle de l'IA dans les efforts de développement durable
Predictive analytics help hospitals reduce waste and optimize energy. For example, a large hospital network using AI to forecast admissions and discharges reduced average length of stay by 0.67 days and achieved cost savings of $55–72 million annually. AI programs like “The Adelaide Score” cut patient stays by 6.5% and saved nearly $10 million annually in Australia.
AI-based risk adjustment models help payers identify high-risk patients, reducing complications and readmissions by 25%, while McKinsey estimates administrative cost reductions up to 25%. AI-driven automation in revenue cycle tasks has also saved 15,000 employee hours per month, halved turnaround times, and generated 30% ROI.
How to Implement AI in Healthcare Industry
Successfully implementing AI in healthcare requires more than just technology, it demands a clear strategy aligned with your organization’s goals and workflows. From assessing readiness to training teams, each step is crucial to unlocking AI’s full potential and achieving meaningful impact.
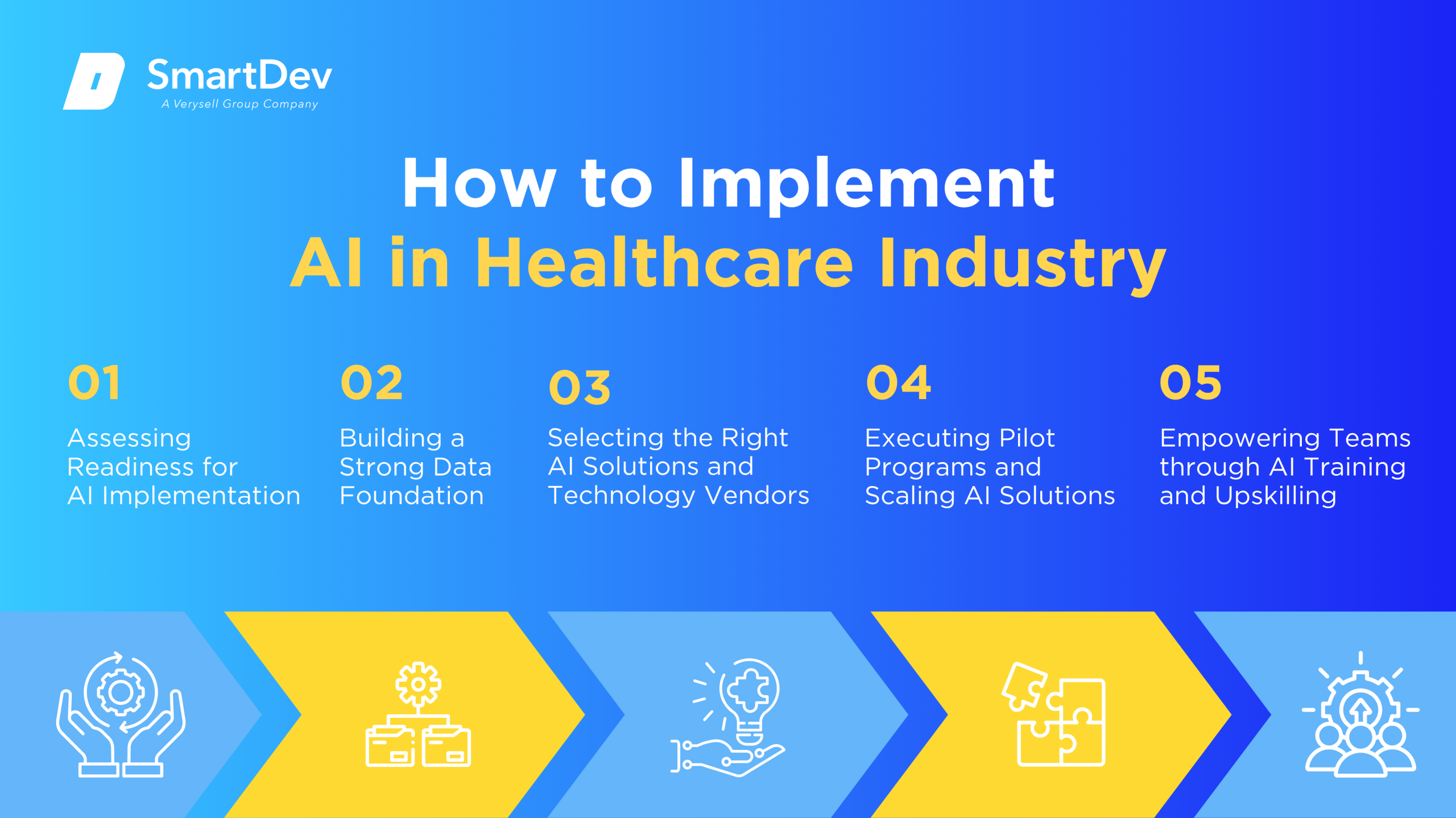
Étape 1 : Évaluer l’état de préparation à l’adoption de l’IA
To begin, healthcare leaders must identify workflows ripe for AI intervention – administrative backlogs, high-cost imaging processes, or chronic care follow-ups. Conduct a readiness assessment: evaluate data quality, IT infrastructure, regulatory compliance needs, and alignment with strategic objectives. Early pilots should target realistic, measurable improvements, such as reducing billing cycle times or waiting list durations.
Mapping existing workflows to AI use cases supports stakeholder engagement. Budgeting early and anticipating change management needs – training, privacy policies, and clinical integration – build a foundation for sustained success.
Étape 2 : Construire une base de données solide
A solid data foundation – the cornerstone of AI – is critical. This involves collecting data from EHRs, imaging systems, billing logs, and remote monitoring devices. Prioritize data cleaning and standardization: accurate timestamps, consistent data formats, and interoperability enable scalable analytics later on.
Data governance isn’t optional – ensure compliance with HIPAA or GDPR, assign ownership and maintenance responsibility. A layered architecture, secure lake or warehouse with controlled access, enables rapid querying by algorithms. Investing now in data quality pays dividends when AI models are deployed.
Strong data infrastructure is key to effective AI. Learn how sound data practices drive smarter decisions in our article on data-driven success.
Étape 3 : Choisir les bons outils et les bons fournisseurs
Select AI platforms tailored to healthcare’s complexity – those that support FDA-cleared models and integrate with workflows. Vendors like Aidoc (for imaging), UiPath (for revenue cycle automation), C2-Ai (for pre‑habilitation), and Mercy’s aiOS bring proven ROI. Evaluate models for transparency, explainability, and clinical validation. Focus on vendors offering secure interfaces with EHRs, mobile tools for clinicians, and implementation support.
A blended approach, using platform providers for core functionality and customized modules for institutional needs, minimizes risk and increases scalability.
Étape 4 : Tests pilotes et mise à l’échelle
Pilot projects let you test hypotheses quickly and measure success before investing heavily. For instance, Mercy’s aiOS radiology deployment was phased gradually across departments. The Adelaide Score trial in Australia rolled out incrementally across wards.
Quando metrics like processing speed, documentation time, patient wait times, and staff satisfaction help demonstrate value. When pilots succeed, deploy in phases, department by department, while maintaining rigorous governance and staff training.
Étape 5 : Former les équipes pour une mise en œuvre réussie
AI is most effective when people understand and trust it. Clinical staff need education on interpreting AI outputs and indicating when they override recommendations. Administrators overseeing automation must be trained on digital workflows and exception handling.
Embed “AI champions” in departments to advocate, guide adoption, and facilitate peer-to-peer learning. Regular update sessions and transparent reporting keep teams engaged. Clarify roles and accountability to avoid “automation surprises” and to promote confidence in AI-human collaborations.
Measuring the ROI of AI in Healthcare Industry
Indicateurs clés pour suivre le succès
Successful ROI measurement blends productivity, cost, quality, and patient outcomes. Productivity gains include clinician-hours freed through documentation automation and faster imaging triage. In administrative domains, UiPath-driven claim automation delivered 15,000 saved hours/month. Quality metrics include reduced length of stay, readmissions, or complications, as seen with the Adelaide Score and Surgery Hero apps.
Financial benefits derive from operational savings: halfic turnaround time, error reduction, and optimized bed usage. Prospective AI risk adjustment models improved coding accuracy to 97.5%, enhanced reimbursements, and cut hospitalizations downstream. Patient-centric benefits: fewer complications, better outcomes, higher satisfaction, enhance ROI indirectly through brand and reimbursement value.
Études de cas démontrant le retour sur investissement
A large US hospital network implemented outcome prediction models across seven hospitals, reducing average stay by nearly 0.7 days per patient. The annual benefit amounted to $55–72 million. The Adelaide Score’s AI-assisted discharge predictions freed beds and saved nearly $10 million annually. C2-Ai’s Surgery Hero app in the UK halved readmission rates and reduced complications six‑fold.
On admin side, Omega Healthcare realized a 30% ROI by automating documentation and claims for 60–70% of clients, saving tens of thousands of hours. These examples prove that when aligned with clear goals, AI investment yields quantifiable returns – financial and clinical.
Pièges courants et comment les éviter
One frequent mistake is treating AI as a checkbox rather than a business strategy. IBM research shows enterprise AI ROI often underperforms expectations, averaging 5.9%, below cost of capital. Avoid this by setting measurable goals, mapping ROI during planning, and integrating continuous performance measurement.
Other pitfalls include lack of data hygiene, unclear stakeholder roles, and failure to secure clinician trust. Tackle these proactively: implement strong data governance, maintain alignment between IT and clinical leadership, and iterate AI models as part of ongoing operations, don’t treat deployment as final.
Future Trends of AI in Healthcare Industry

Prévisions pour la prochaine décennie
Over the next decade, AI in healthcare will evolve from diagnostics and automation toward predictive and prescriptive analytics that power personalized and preventive care. The shift will be driven by increasing investments – both public and private. Expect to see AI deeply embedded in clinical decision-making, real-time remote patient monitoring, and hyper-personalized treatment planning.
As adoption grows, healthcare systems will also need to formalize governance frameworks to ensure AI is used safely and ethically. Technologies like federated learning and explainable AI will become the norm, especially as regulatory bodies push for greater transparency. Certification models tailored to healthcare AI will help standardize deployment in electronic health records and medical devices across institutions.
Comment les entreprises peuvent garder une longueur d'avance
To stay ahead, healthcare organizations must invest in data infrastructure, ensuring systems are interoperable, secure, and optimized for AI integration. A robust data-first approach enables smoother AI adoption and helps drive real-time insights at scale. Partnering with both established vendors and nimble AI startups will also provide access to cutting-edge solutions with proven value.
Equally important is staying informed on evolving regulations, reimbursement models, and emerging AI safety standards. Cultivating trust among clinicians and patients through transparent processes and consistent engagement will smooth the path to adoption. Ultimately, businesses that proactively shape AI strategy today will become the leaders of tomorrow’s healthcare transformation.
Conclusion
Principaux points à retenir
AI is already reshaping healthcare by delivering clear improvements in diagnostics, administrative efficiency, and patient monitoring. From reducing hospital stays to enhancing accuracy in billing and coding, organizations are seeing real financial and clinical returns. The success of these initiatives, however, hinges on aligning AI projects with strategic goals and maintaining robust governance structures.
Healthcare leaders must recognize that AI isn’t a one-off investment, it’s an ongoing transformation that requires commitment and adaptability. Measurable ROI comes from smart implementation, data readiness, and continuous evaluation. When executed thoughtfully, AI has the power to elevate patient care, streamline operations, and deliver long-term value.
Moving Forward: A Strategic Approach to AI-Driven Transformation
As AI redefines the healthcare ecosystem, organizations have a critical opportunity to improve clinical outcomes, streamline operations, and unlock new efficiencies across the care continuum. From predictive diagnostics and personalized treatment planning to automated administrative workflows and real-time patient monitoring, integrating AI is rapidly becoming a strategic imperative for future-ready healthcare systems.
At SmartHealth AI, we develop tailored AI solutions that empower providers to optimize decision-making, reduce operational burdens, and enhance patient experiences. Whether you’re deploying intelligent automation to reduce claim denials or integrating predictive analytics to manage population health, our experts work closely with your teams to deliver scalable, compliant, and outcomes-driven systems.
Explore how SmartDev delivers AI-powered solutions across diagnostics, automation, and care delivery on our Soins de santé et services médicaux page.
—
Références:
- AI In Healthcare Stats 2025: Adoption, Accuracy & Market | DemandSage
- AI isn’t replacing radiologists. Instead, they’re using it to tackle time-sucking administrative tasks | Business Insider
- Why AI May Be Listening In on Your Next Doctor’s Appointment | The Wall Street Journal
- Driving the Future of Health with AI | Healthcare Information and Management Systems Society
- Remote patient monitoring using artificial intelligence: Current state, applications, and challenges | arXiv
- Is AI in Medicine Playing Fair? | Mount Sinai
- Custom Prostate Cancer Treatment: ArteraAI Multimodal Artificial Intelligence | Time Magazine
- The future of healthcare using multimodal AI: Technology that can read, see, hear and sense | Oral Oncology Reports
- Measuring the Cost and Return on Investment (ROI) with AI Implementation | BHM Healthcare Solutions
- Patient Outcome Predictions Improve Operations at a Large Hospital Network | arXiv








