Introduction
Radiology is at a crossroads—demand for imaging services continues to grow while radiologists face mounting workloads, increasing complexity of cases, and pressure to deliver faster, more accurate diagnoses. Artificial Intelligence (AI) is emerging as a game-changer, enhancing diagnostic precision, streamlining workflows, and enabling earlier detection of disease.
This in-depth guide explores the most impactful AI use cases in radiology, outlining real-world benefits, measurable trends, and the challenges to adoption.
What is AI and Why Does It Matter in Radiology?
 Definition of AI and Its Core Technologies
Definition of AI and Its Core Technologies
Artificial Intelligence (AI) refers to computer systems designed to perform tasks that typically require human intelligence, such as pattern recognition, decision-making, and natural language understanding. Core technologies include machine learning, natural language processing, and computer vision.
In radiology, AI applies these technologies to interpret medical images, detect anomalies, quantify disease progression, and integrate imaging data with other clinical information. The aim is not to replace radiologists, but to augment their capabilities—helping them work faster and more accurately.
Want to explore how AI can transform your sector? Discover real-world strategies for deploying smart technologies in your sector. Visit How to Integrate AI into Your Business in 2025 to get started today and unlock the full potential of AI for your business!
The Growing Role of AI in Transforming Radiology
AI is fundamentally changing how radiology departments operate. Algorithms trained on large datasets of annotated images can detect abnormalities—such as lung nodules, brain hemorrhages, or bone fractures—within seconds, acting as a “second pair of eyes” for radiologists.
Workflow orchestration tools are using AI to prioritize urgent cases in the reading queue, ensuring patients with critical conditions are diagnosed and treated sooner.
AI is also facilitating precision medicine by integrating imaging biomarkers with genomics, lab results, and electronic health records, enabling more personalized treatment planning.
Key Statistics or Trends in AI Adoption
The adoption curve is accelerating. According to a 2023 Grand View Research report, the AI in medical imaging market is projected to reach USD 20.9 billion by 2030, growing at a CAGR of 36.9%.
A 2022 RSNA survey found that over 30% of radiology practices in the U.S. had implemented some form of AI in their workflows, with the majority reporting improvements in report turnaround times.
Early detection impact is also compelling—Nature Medicine published a study showing that an AI breast cancer detection model outperformed human radiologists in reducing both false positives and false negatives.
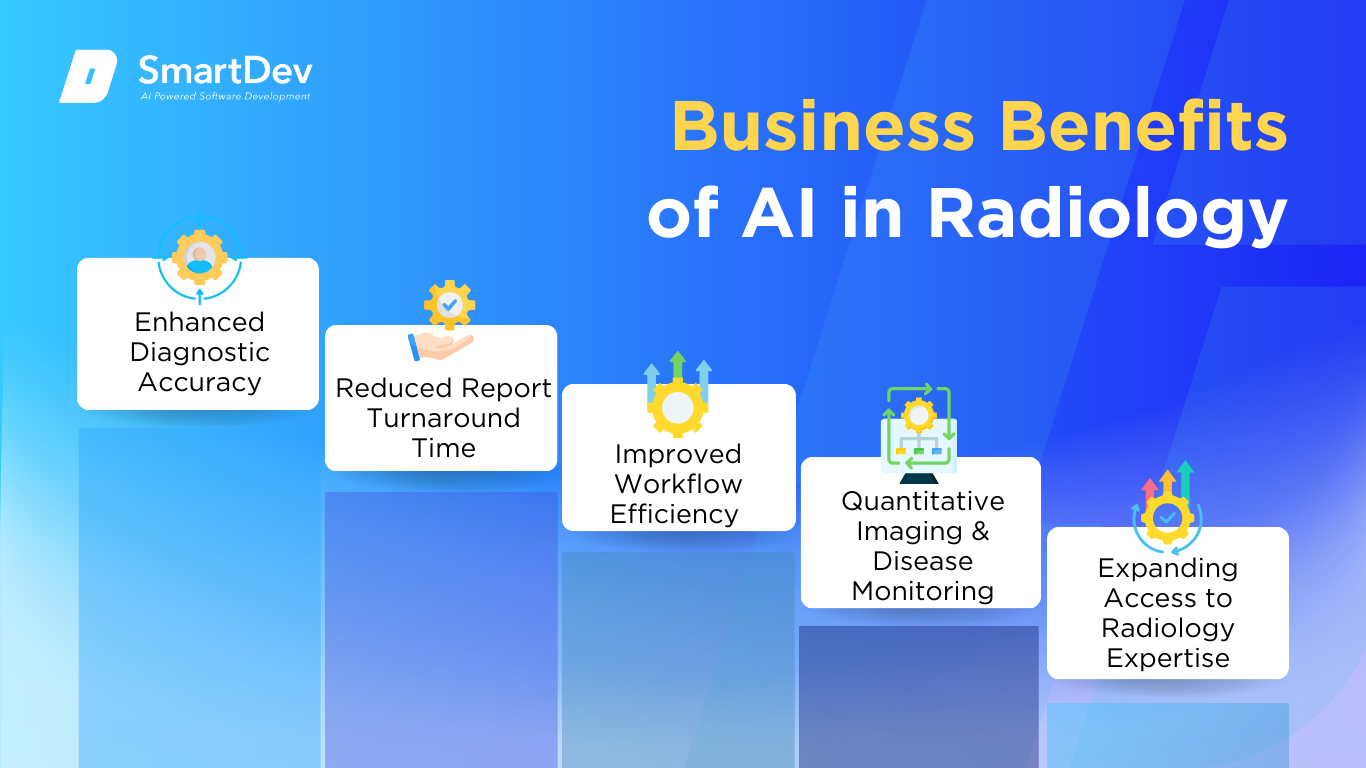
Business Benefits of AI in Radiology
1. Enhanced Diagnostic Accuracy
Radiologists handle an overwhelming volume of studies daily, ranging from routine X-rays to complex MRI scans. Human fatigue, variability in training, and time pressure can lead to missed subtle findings, particularly in early-stage disease. AI algorithms trained on millions of annotated cases can act as an always-alert assistant, scanning images for patterns consistent with pathology.
For example, Google Health’s AI model for breast cancer detection demonstrated reduced false positives and false negatives compared to radiologists working alone. In stroke care, AI-driven CT perfusion analysis tools can identify ischemic areas within minutes, enabling earlier intervention and better outcomes. This increase in sensitivity and specificity is not about replacing radiologists but empowering them with a safety net that consistently catches what might be missed.
2. Reduced Report Turnaround Time
Delays in radiology reports can bottleneck treatment decisions, particularly in emergency medicine where every minute counts. AI can preprocess studies by automatically detecting, tagging, and even drafting key findings before the radiologist opens the case.
Hospitals using AI-powered chest X-ray triage tools have cut time-to-diagnosis for conditions like pneumothorax from several hours to under 15 minutes. This acceleration is critical in trauma, stroke, and cardiac emergencies where time-sensitive interventions can determine patient survival rates.
3. Improved Workflow Efficiency
Radiology workflows often involve manual sorting, assigning cases to specialists, and switching between multiple systems for PACS, RIS, and EHR. AI-driven workflow orchestration automates these processes, ensuring urgent cases jump to the top of the list, studies are routed to subspecialists, and all relevant prior exams are automatically retrieved.
This reduces administrative workload and cognitive switching costs for radiologists, enabling them to devote more time to complex case interpretation. The downstream effect includes fewer reporting errors, more consistent turnaround times, and better interdepartmental coordination—ultimately boosting departmental productivity without additional headcount.
4. Quantitative Imaging and Disease Monitoring
Longitudinal tracking of disease progression is a cornerstone of radiology in oncology, neurology, and cardiology. Manually measuring lesions or comparing sequential scans is time-consuming and prone to variability. AI tools perform precise image segmentation, volume quantification, and texture analysis in seconds, offering consistent and reproducible metrics.
In oncology, volumetric tumor analysis supported by AI not only aids treatment planning but also accelerates clinical trial assessments by providing objective endpoints. Neurology departments use AI-powered volumetric analysis to monitor neurodegenerative diseases such as Alzheimer’s, detecting changes years before they become clinically apparent.
5. Expanding Access to Radiology Expertise
Globally, there is a shortage of radiologists, with rural and low-resource areas particularly affected. AI can serve as a first-pass screening solution, flagging potentially abnormal studies for priority review by human specialists.
Tele-radiology providers are already leveraging AI to prescreen large volumes of images, ensuring that urgent cases from remote hospitals are escalated within minutes. In LMICs (low- and middle-income countries), portable imaging devices paired with AI analysis are helping clinicians identify tuberculosis or pneumonia in settings without an on-site radiologist, thereby narrowing the healthcare access gap.
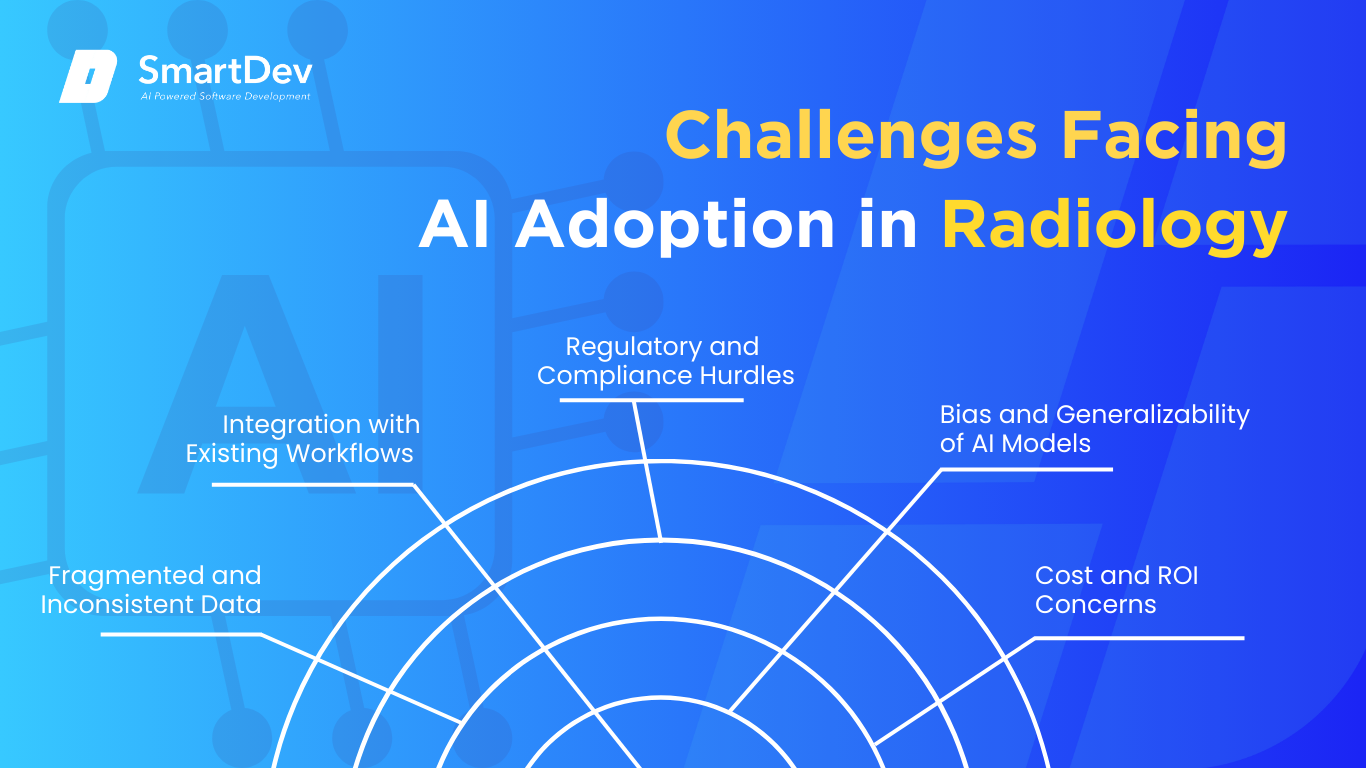
Challenges Facing AI Adoption in Radiology
 1. Fragmented and Inconsistent Data
1. Fragmented and Inconsistent Data
Radiology AI models require massive amounts of high-quality, standardized imaging data for training and validation. In reality, imaging protocols vary by scanner manufacturer, hospital, and even operator, leading to inconsistencies in resolution, contrast, and annotations. These differences can degrade AI performance when models are deployed outside of their training environment.
Addressing this requires industry-wide adherence to standards like DICOM and structured reporting templates, as well as investments in data cleaning pipelines that harmonize heterogeneous datasets without losing clinically relevant detail.
Siloed systems and scattered data can cripple decision-making and slow growth. Discover how AI is helping organizations unify, clean, and unlock value from their data faster and smarter. Explore the full article to see how AI transforms data chaos into clarity.
2. Integration with Existing Workflows
Even the most accurate AI model can fail commercially if it disrupts how radiologists work. Solutions that require extra clicks, separate log-ins, or manual data transfers slow down users instead of helping them.
To achieve adoption, AI must integrate seamlessly into PACS, RIS, and EHR systems, presenting insights in the same viewer radiologists already use. This often requires collaboration between AI vendors, IT departments, and clinical leadership to customize deployments for each institution’s infrastructure.
3. Regulatory and Compliance Hurdles
AI in medical imaging is subject to strict regulatory oversight to ensure patient safety and clinical efficacy. In the U.S., tools must secure FDA 510(k) clearance or De Novo classification, which can be a multi-year process involving extensive validation studies.
In the EU, compliance with the MDR (Medical Device Regulation) adds another layer of complexity. Smaller AI startups may lack the resources for these regulatory pathways, slowing market entry and innovation.
4. Bias and Generalizability of AI Models
If a model is trained primarily on datasets from a specific geographic region, demographic group, or scanner type, it may underperform when applied to different populations. For example, an AI model trained on predominantly adult data may fail to accurately interpret pediatric scans.
Bias not only risks patient harm but also undermines clinician trust. Continuous model retraining with diverse datasets, rigorous external validation, and transparent performance reporting are essential to ensure equitable care.
For those navigating these complex waters, a business-oriented guide to responsible AI and ethics offers practical insights on deploying AI responsibly and transparently, especially when public trust is at stake.
5. Cost and ROI Concerns
Implementing AI involves more than purchasing software—it may require GPU-enabled servers, secure cloud storage, integration services, and ongoing maintenance. For many hospitals operating on tight margins, the upfront and recurring costs can be a barrier.
Demonstrating ROI requires quantifying both direct gains (e.g., reduced reporting time, improved accuracy) and indirect benefits (e.g., fewer readmissions, higher patient throughput). Institutions that can link AI adoption to measurable clinical and operational improvements will have a stronger case for investment.
Specific Applications of AI in Radiology
 Use Case 1: Automated Image Analysis and Diagnosis
Use Case 1: Automated Image Analysis and Diagnosis
AI’s ability to process and analyze medical images at scale is one of its most transformative applications in radiology. Machine learning algorithms, particularly deep learning, are used to identify patterns in medical images that may not be immediately apparent to the human eye. These algorithms are trained on vast datasets of medical images to identify conditions such as tumors, fractures, and neurological abnormalities.
AI-powered image analysis helps radiologists quickly detect and diagnose conditions, reducing the time it takes to provide results to patients. This capability significantly improves workflow efficiency, allowing radiologists to focus on more complex cases. It also helps reduce the potential for human error, ensuring higher diagnostic accuracy, especially in regions with limited access to specialist radiologists.
However, implementing AI in image analysis also raises concerns related to data privacy, model bias, and the integration of AI tools into existing hospital workflows. The adoption of AI systems requires comprehensive validation to ensure that the models perform well across diverse patient populations and medical conditions.
Real-World Example
Aidoc, a leading provider of AI-based diagnostic tools for radiologists, developed a platform that assists in the rapid analysis of CT scans. The platform’s AI algorithms are designed to identify life-threatening conditions, such as brain hemorrhages, in real-time. Aidoc’s technology has been shown to reduce the time to diagnosis, improving clinical outcomes and enabling faster intervention. In a study, Aidoc’s AI system demonstrated a 20% reduction in the time to diagnosis for intracranial hemorrhage, potentially saving lives.
Use Case 2: AI-Driven Workflow Optimization
AI technologies are being used to streamline the radiology workflow by automating repetitive tasks such as image sorting, reporting, and prioritization of cases. AI can categorize images based on urgency, ensuring that critical cases are prioritized for review by radiologists. It can also generate preliminary reports that radiologists can refine, saving time and improving accuracy.
Workflow optimization through AI reduces administrative burden and minimizes delays in diagnosis and treatment. By automating routine tasks, AI frees up radiologists to spend more time on complex cases that require human expertise. This application of AI also enhances productivity in departments that are under pressure due to high volumes of cases.
Despite the clear benefits, integrating AI into existing radiology workflows requires a robust IT infrastructure and careful consideration of human factors, such as radiologist trust in the technology and the ease of adoption.
Real-World Example
Zebra Medical Vision uses AI to automate the process of analyzing medical images and prioritizing cases. Their platform integrates with existing Picture Archiving and Communication Systems (PACS) to quickly categorize images and provide radiologists with insights. Zebra’s AI solution has been shown to increase radiologist productivity by enabling faster image review and more accurate reporting. In one case, their AI tool helped reduce the time to diagnosis for lung disease by 30%.
Use Case 3: AI in Predictive Analytics for Patient Outcomes
AI’s predictive capabilities are being used in radiology to forecast patient outcomes based on imaging data. By analyzing trends in medical imaging alongside patient health data, AI can predict the progression of diseases such as cancer or cardiovascular conditions. This predictive analysis helps clinicians plan more effective treatment strategies and improves long-term patient care.
AI-powered predictive tools also support early intervention by identifying patients at high risk of developing severe conditions. By identifying these risks early, healthcare providers can initiate preventative measures, improving patient outcomes and reducing the burden on the healthcare system.
However, predictive models need to be carefully validated and continuously updated to reflect changes in medical trends and patient demographics.
Real-World Example
In collaboration with the UK’s National Health Service (NHS), Google Health developed an AI system for breast cancer screening. The system uses mammography images to predict the likelihood of a positive diagnosis, improving early detection rates. In clinical trials, the AI system outperformed human radiologists, reducing false positives by 5.7% and false negatives by 9.4%. This system’s predictive power allows for more accurate screening, leading to better early intervention and improved patient outcomes.
Use Case 4: Personalized Treatment Recommendations
AI is playing a key role in personalizing treatment plans for patients based on medical imaging and other clinical data. AI algorithms can analyze a patient’s medical history, genetic data, and imaging results to provide tailored treatment recommendations. This ensures that treatment plans are not only based on generic protocols but are also aligned with the specific needs of the patient.
By providing personalized recommendations, AI can improve the precision of radiological interventions, ensuring that patients receive the most appropriate treatments for their conditions. This application is particularly valuable in complex cases such as cancer, where personalized care plans are crucial to optimizing outcomes.
One challenge with this application is the need for high-quality, standardized data across different healthcare systems to train AI models effectively.
Real-World Example
PathAI, a provider of AI-powered diagnostic tools, developed a system that uses medical images to recommend personalized treatment plans for cancer patients. By analyzing pathology slides, the AI tool can predict how a cancer will respond to specific treatments, helping doctors tailor their approach to the individual patient. In clinical trials, PathAI’s system improved treatment response rates by 15%, demonstrating the power of AI in personalized cancer care.
Use Case 5: AI-Assisted Radiology Reporting
Radiologists are using AI to generate structured reports from medical imaging data. AI systems are trained to identify key features in images, such as the size and location of tumors, and automatically generate text-based reports. These systems can also flag potential issues or discrepancies, ensuring that nothing is overlooked in the reporting process.
This use of AI enhances report accuracy and reduces the risk of errors, which is crucial in fast-paced environments where radiologists are dealing with large volumes of images. It also helps standardize reports across different institutions, ensuring consistency in diagnosis.
While AI-generated reports have been shown to improve accuracy, the integration of AI into the reporting process requires careful consideration of data privacy and cybersecurity concerns.
Real-World Example
Qure.ai’s AI technology assists radiologists by generating automated reports for CT scans, X-rays, and MRIs. The platform analyzes medical images and creates a detailed report, highlighting key findings such as abnormal growths or fractures. Qure.ai’s system has reduced report generation times by 40% and has improved diagnostic accuracy by helping radiologists spot subtle anomalies that may have been missed in traditional review processes.
Use Case 6: AI in Radiology Education and Training
AI is being utilized in radiology education to train medical professionals. AI-driven simulation tools can mimic real-world clinical scenarios, allowing radiology students to practice interpreting medical images in a controlled environment. These tools offer immediate feedback and help students learn more efficiently.
AI-powered education platforms are designed to enhance the learning experience by providing personalized feedback based on a learner’s performance. By using AI in education, radiology programs can ensure that students are better prepared to handle real-world cases upon graduation.
As with other AI applications in healthcare, ethical considerations regarding the accuracy of training data and the reliability of AI-driven feedback must be addressed.
Real-World Example
Radiology Mastery uses AI to create interactive learning modules for radiology students. The AI system analyzes student responses and provides personalized recommendations for improvement. This technology has been shown to enhance learning outcomes by 25%, as students receive immediate feedback and are able to focus on areas where they need the most improvement.
Need Expert Help Turning Ideas Into Scalable Products?
Partner with SmartDev to accelerate your software development journey — from MVPs to enterprise systems.
Book a free consultation with our tech experts today.
Let’s Build TogetherExamples of AI in Radiology
Real-World Case Studies
 Aidoc: AI-Assisted Emergency Radiology
Aidoc: AI-Assisted Emergency Radiology
Aidoc has revolutionized emergency radiology with AI tools that automatically analyze CT scans to detect critical conditions such as intracranial hemorrhages. Their system reduces the time to diagnosis, allowing for faster treatment and improving patient outcomes. The tool has been adopted in over 300 hospitals, where it has reduced time to diagnosis by 20%, improving clinical response time in life-threatening situations.
Zebra Medical Vision: AI for Early Disease Detection
Zebra Medical Vision’s AI platform analyzes medical images to detect a variety of conditions, from cardiovascular disease to cancer. Their AI tool integrates with hospital PACS systems, providing immediate analysis to speed up diagnosis and treatment. Zebra’s AI system has been shown to improve diagnostic accuracy, leading to a 30% reduction in false negatives for certain conditions.
Google Health: AI in Breast Cancer Screenin
Google Health’s collaboration with the NHS demonstrated the power of AI in improving breast cancer screening. Their AI model outperformed human radiologists in both reducing false positives and false negatives, improving early detection and diagnosis. This advancement has the potential to revolutionize breast cancer screening, making it more accurate and less invasive.
These examples reflect the value of working with technology partners who understand both the technical and policy implications. If you’re considering a similar digital transformation, don’t hesitate to connect with AI implementation experts to explore what’s possible in your context.
Innovative AI Solutions
AI-Powered Radiology Assistants
Emerging AI solutions are integrating assistant capabilities into radiology workflows. These AI-powered assistants can suggest potential diagnoses, review reports, and even generate initial interpretations, allowing radiologists to make faster and more accurate decisions. The introduction of AI assistants is poised to redefine the role of radiologists, making their work more efficient and less prone to error.
Deep Learning for Tumor Detection
Deep learning technologies are pushing the boundaries of tumor detection in medical imaging. By training on vast datasets of radiology images, deep learning models are becoming adept at detecting even the smallest abnormalities in CT scans, MRIs, and X-rays. These models are expected to significantly improve the early detection of various types of cancer, offering the potential for life-saving interventions.
AI-Driven Predictive Analytics for Patient Risk
AI’s predictive capabilities are advancing patient care in radiology by forecasting potential complications based on imaging data. This technology is being used to predict patient outcomes for conditions such as cardiovascular diseases and cancers, improving treatment planning and preventative care strategies. By enabling early interventions, AI-driven predictive analytics is reducing healthcare costs and improving patient quality of life.
In conclusion, AI use cases in radiology are not just improving diagnostic accuracy and efficiency—they are transforming the entire healthcare landscape. As AI technologies continue to evolve, they will further shape how radiologists diagnose, treat, and manage patient care, making radiology a key area for innovation in the healthcare sector.
AI-Driven Innovations Transforming Radiology
Emerging Technologies in AI for Radiology
AI technologies, especially machine learning and deep learning, have made remarkable strides in radiology. Generative AI is one of the key advancements, allowing for the generation of synthetic medical images for training AI models, improving data availability, and augmenting radiologists’ diagnostic capabilities. Computer vision, another breakthrough in AI, is empowering radiologists to analyze visual data at an unprecedented scale and accuracy, helping them identify abnormalities and detect diseases in the early stages.
AI-powered solutions now support advanced diagnostic tools that detect conditions such as cancers, fractures, cardiovascular diseases, and neurological abnormalities from medical imaging. These AI tools not only enhance the efficiency of imaging analysis but also reduce the workload on radiologists, allowing them to focus on more complex cases that require human expertise. The integration of AI into radiology practices brings the promise of more personalized and faster care for patients.
AI’s Role in Sustainability Efforts
As healthcare systems globally strive for greater sustainability, AI plays a crucial role in reducing the environmental footprint of radiology departments. One significant application is predictive analytics, which helps in the optimization of resources and reducing waste. By analyzing imaging workflows and predicting patient needs, AI can help hospitals optimize scheduling and reduce unnecessary tests, ensuring that imaging resources are used more efficiently.
AI also plays a pivotal role in optimizing energy consumption within radiology departments. Smart systems powered by AI can dynamically adjust energy usage based on patient volume and equipment requirements, leading to more sustainable operations. The integration of AI into the energy management of radiology departments can lower operational costs, reduce carbon footprints, and contribute to the broader sustainability goals of healthcare organizations.
How to Implement AI in Radiology
 Step 1: Assessing Readiness for AI Adoption
Step 1: Assessing Readiness for AI Adoption
Before diving into AI integration, it’s essential for radiology departments to assess their readiness for AI adoption. Identifying the areas within a radiology department that can benefit from AI is the first step. Tasks such as image analysis, report generation, and diagnostic support are prime candidates for AI integration. Furthermore, considering the organization’s data infrastructure and the ability to process vast amounts of medical imaging data is crucial in this evaluation.
Successful AI adoption also requires alignment with overall healthcare goals and a clear understanding of the expected outcomes, such as reduced diagnostic time and improved accuracy. For healthcare providers, adopting AI can be a significant shift in workflows, and ensuring the readiness of the department is essential for smooth integration.
Step 2: Building a Strong Data Foundation
AI in radiology heavily depends on quality data. To ensure the effectiveness of AI tools, radiology departments must focus on collecting, cleaning, and managing imaging data efficiently. This includes gathering diverse datasets from various imaging modalities and ensuring that data is labeled accurately to facilitate machine learning model training.
Data management best practices include creating centralized data repositories, establishing protocols for data security, and ensuring compliance with healthcare regulations such as HIPAA. By investing in robust data management systems, healthcare organizations can lay a solid foundation for AI adoption, enhancing the reliability and performance of AI tools.
Step 3: Choosing the Right Tools and Vendors
Selecting the right AI tools and vendors is critical for successful implementation. Radiology departments need to evaluate AI platforms that align with their specific needs, whether it’s automating image analysis, supporting clinical decision-making, or enhancing workflow efficiency. It’s essential to choose AI solutions that integrate seamlessly with existing radiology systems such as Picture Archiving and Communication Systems (PACS).
Vetting potential vendors based on their experience in the healthcare sector, their ability to meet regulatory standards, and the performance metrics of their AI solutions is key. Furthermore, ensuring that the AI solutions are scalable and adaptable to future needs can help future-proof the department’s investment in AI technologies.
Step 4: Pilot Testing and Scaling Up
Before fully deploying AI across a radiology department, conducting small-scale pilot tests is crucial. These pilot tests allow healthcare organizations to assess the AI solution’s performance in real-world settings, identify potential issues, and measure the impact of AI on workflow efficiency. By starting with a smaller test group, radiology departments can gather feedback from radiologists and other stakeholders, making necessary adjustments before full-scale implementation.
Once the pilot phase is successful, scaling up AI adoption across the department becomes easier. Continuous monitoring and adjusting the deployment ensure that AI tools are working optimally and delivering the desired results, such as faster image analysis and improved diagnostic accuracy.
Step 5: Training Teams for Successful Implementation
A successful AI implementation in radiology depends not only on the technology but also on the radiologists and healthcare professionals who use it. Upskilling and training teams to work alongside AI technologies is crucial for maximizing the benefits of AI in the department. Training should focus on how AI tools complement traditional radiology workflows and enhance diagnostic decision-making rather than replace human expertise.
Providing ongoing education and resources will help radiologists feel comfortable using AI systems and foster collaboration between AI technology and healthcare professionals. Building trust in AI is essential for its successful integration into the radiology practice.
Whether you’re exploring your first pilot or scaling an enterprise-wide solution, our team is here to help. Get in touch with SmartDev and let’s turn your challenges into opportunities.
Measuring the ROI of AI in Radiology
Key Metrics to Track Success
To evaluate the success of AI adoption in radiology, organizations must track key performance metrics. Productivity improvements, such as reduced time spent per image analysis, and diagnostic accuracy are critical indicators of AI’s impact. By automating routine tasks such as image sorting and report generation, AI frees up valuable time for radiologists, enabling them to focus on more complex cases.
Cost savings achieved through automation also contribute significantly to ROI. AI can reduce operational costs by eliminating the need for manual processes, optimizing resource allocation, and improving operational efficiency. These savings can then be reinvested into further AI development or expansion, creating a sustainable cycle of improvement.
Case Studies Demonstrating ROI
Several organizations have already realized significant ROI from integrating AI into their radiology practices. For instance, Aidoc’s AI system has proven to be a game-changer in emergency radiology, reducing the time to diagnose life-threatening conditions by 20%. The faster diagnosis translates into quicker interventions and better patient outcomes, ultimately improving the hospital’s bottom line by streamlining the treatment process and enhancing patient throughput.
Another example is Zebra Medical Vision, whose AI-powered platform has improved the accuracy and speed of diagnosing cardiovascular and pulmonary conditions. By automating image interpretation, Zebra’s system has reduced diagnostic errors and improved overall patient care. The financial benefits of these improvements are realized in reduced patient readmissions and lower treatment costs.
Common Pitfalls and How to Avoid Them
While AI adoption in radiology offers numerous benefits, there are also common pitfalls that organizations must be mindful of. One major challenge is ensuring data quality. Poor-quality or incomplete data can undermine the effectiveness of AI tools, leading to inaccurate diagnoses and unreliable results. To avoid this, radiology departments must invest in data management and validation processes to ensure that the AI models are trained on high-quality, comprehensive datasets.
Another pitfall is resistance from radiologists and other healthcare professionals. AI implementation can be met with skepticism, particularly if there’s a perceived threat to job security. To overcome this challenge, organizations should focus on education and transparent communication about how AI will support, rather than replace, human expertise in the diagnostic process.
Understanding ROI is possibly a challenge to many businesses and institutions as different in background, cost. So, if you need to dig deep about this problem, you can read AI Return on Investment (ROI): Unlocking the True Value of Artificial Intelligence for Your Business
Future Trends of AI in Radiology
 Predictions for the Next Decade
Predictions for the Next Decade
The next decade promises exciting advancements in AI for radiology, particularly in the areas of personalized medicine and predictive diagnostics. AI models will continue to evolve, becoming even more sophisticated at identifying patterns and trends within medical images. These advancements will lead to more accurate early diagnoses, personalized treatment plans, and improved patient outcomes.
Moreover, AI will increasingly be integrated into radiology education, helping to train future radiologists more efficiently. As AI technologies become more advanced, they will not only assist with diagnostics but also actively guide treatment decisions, making radiology an even more integral part of patient care.
How Businesses Can Stay Ahead of the Curve
To stay ahead of the curve in AI adoption, radiology departments must continue to innovate and invest in emerging AI technologies. By partnering with AI vendors, healthcare providers can gain early access to cutting-edge tools and stay competitive in the rapidly evolving healthcare landscape. Additionally, ongoing research and development will be critical in ensuring that AI tools remain effective and aligned with the latest medical advancements.
Building a culture of innovation within the radiology department will also help businesses adapt to new AI developments. Encouraging collaboration between AI specialists, radiologists, and healthcare providers can foster an environment where AI technologies are continuously improved and optimized for better patient care.
Conclusion
Summary of Key Takeaways on AI Use Cases in Radiology
AI has immense potential to transform radiology, improving diagnostic accuracy, operational efficiency, and patient care. From AI-driven image analysis to predictive analytics, the applications of AI in radiology are vast and diverse. By adopting AI, radiology departments can enhance their workflows, reduce errors, and provide more timely diagnoses, all while optimizing resource allocation and reducing costs.
Moving Forward: A Path to Progress for Businesses Considering AI Adoption
If you are considering implementing AI in your radiology department, now is the time to explore the possibilities. Start by assessing your readiness, investing in a robust data foundation, and choosing the right AI solutions that align with your organizational needs. With AI driving innovation in radiology, those who embrace these technologies will be positioned at the forefront of the industry, delivering improved care and driving greater operational success.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10487271/
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10487271/
- https://www.sciencedirect.com/science/article/abs/pii/S0720048X2400514X
- https://news.northwestern.edu/stories/2025/06/new-ai-transforms-radiology-with-speed-accuracy-never-seen-before/
- https://www.thelancet.com/journals/ebiom/article/PIIS2352-3964(24)00471-7/fulltext
- https://pubs.rsna.org/journal/ai


 1. Fragmented and Inconsistent Data
1. Fragmented and Inconsistent Data Use Case 1: Automated Image Analysis and Diagnosis
Use Case 1: Automated Image Analysis and Diagnosis Aidoc: AI-Assisted Emergency Radiology
Aidoc: AI-Assisted Emergency Radiology 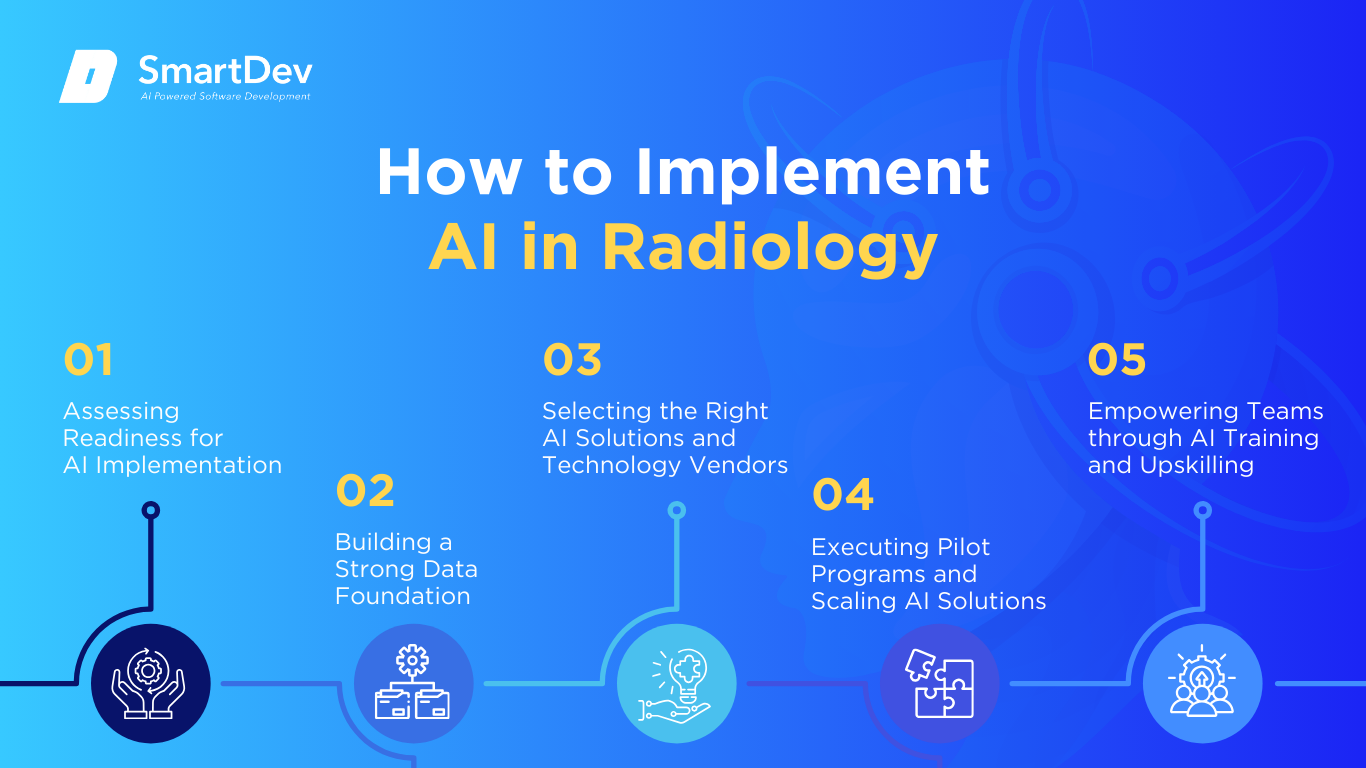 Step 1: Assessing Readiness for AI Adoption
Step 1: Assessing Readiness for AI Adoption Predictions for the Next Decade
Predictions for the Next Decade





