Introduction
Healthcare is at a breaking point. Rising patient volumes, clinician burnout, and soaring operational costs are overwhelming systems around the world. AI in medicine is no longer experimental; it is a proven tool actively reshaping diagnostics, treatment planning, clinical operations, and patient engagement. This in-depth guide explores how AI is transforming modern medicine, unlocking new efficiencies, and paving the way for more personalized, proactive, and accessible care.
What is AI and Why Does It Matter in Medicine?

Definition of AI and Its Core Technologies
AI refers to technologies that mimic human cognitive functions such as learning, reasoning, decision-making, and pattern recognition. In medicine, core AI technologies include machine learning for predictive analytics, natural language processing (NLP) for analyzing clinical texts, computer vision for interpreting medical images, and generative AI for automating documentation and summarization.
AI enables physicians to make faster and more accurate clinical decisions. From flagging abnormalities in radiology scans within seconds to drafting discharge summaries and powering 24/7 virtual care agents, AI is addressing critical pain points in medicine, reducing delays, enhancing diagnostic accuracy, and expanding access to care.
The Growing Role of AI in Transforming Medicine
AI is fundamentally changing how medicine is practiced, from diagnosis and documentation to treatment optimization and patient communication. In imaging, platforms like Aidoc and Viz.ai use computer vision to detect strokes, pulmonary embolisms, and tumors in real time, reducing critical decision times and improving emergency outcomes.
Clinical documentation is also evolving. Generative AI tools are enabling ambient scribing by capturing and structuring doctor-patient conversations, cutting note-taking time by more than half. Health systems like Stanford Health Care and HCA Healthcare are piloting AI copilots that support everything from decision-making to billing.
Patient engagement is entering a new era. AI-powered chatbots are delivering accurate triage, answering health questions, and guiding patients through follow-up care, all without human intervention. These tools not only improve patient satisfaction but also reduce workload for frontline clinicians.
Key Statistics and Trends in AI Adoption in Medicine
AI is becoming integral to clinical medicine. According to the American Medical Association’s 2024 survey on augmented intelligence, 66% of physicians were using AI tools in their practice—up from just 38% the previous year. Key use cases include diagnostic support, radiology interpretation, personalized treatment recommendations, and real-time clinical documentation.
Specialty adoption is also accelerating. In radiology, 90% of large medical groups have integrated AI tools for image analysis, detecting abnormalities like tumors, strokes, and fractures faster and more accurately than traditional methods. In oncology and pathology, AI-driven tools are enhancing decision-making by classifying cancer types, predicting treatment response, and optimizing biopsy interpretations.
The clinical AI market is expanding alongside demand. TempDev reports that the global market for AI in medical diagnostics and treatment is projected to exceed $200 billion by 2030, driven by breakthroughs in generative AI, multimodal diagnostics, and personalized therapeutics. As medical workloads intensify, AI is helping physicians make faster, safer, and more data-informed decisions at the point of care.
Business Benefits of AI in Medicine
AI is transforming the medical field by solving long-standing clinical pain points. From the clinic to the lab, AI is enabling physicians to make faster, more accurate, and data-driven decisions. Below are five core business benefits of integrating AI into modern medical workflows:

1. Accelerated Diagnostics and Clinical Decision Support
AI enhances diagnostic accuracy and speed by interpreting medical imaging, pathology slides, and clinical data in near real-time. Tools now can detect acute conditions such as intracranial hemorrhages or pulmonary embolisms in under five minutes, prompting faster physician response and reducing the risk of missed diagnoses.
Beyond imaging, AI-powered decision support tools analyze patient histories, labs, and vitals to recommend diagnostic pathways and flag deteriorating patients. Systems at institutions like Mayo Clinic now identify early signs of sepsis or cardiac failure before symptoms escalate, allowing for earlier interventions and fewer complications.
2. Personalized Treatment Planning
AI enables more precise and individualized treatment strategies by integrating genomic, imaging, and clinical data. In oncology, platforms like Tempus and IBM Watson for Oncology recommend therapies based on a patient’s tumor profile, clinical stage, and published literature, helping oncologists tailor treatment beyond standard protocols.
In chronic disease management, AI models predict how patients will respond to specific drug regimens. For example, in diabetes care, machine learning algorithms can anticipate glycemic variability and suggest optimal insulin dosages, improving outcomes while reducing adverse events.
3. Enhanced Efficiency in Clinical Documentation
Generative AI tools are significantly reducing the administrative burden of medical documentation. Ambient scribing solutions like Suki and Nuance DAX automatically transcribe physician-patient conversations and generate structured clinical notes, cutting documentation time by more than 50%.
This frees up physicians to spend more time with patients while reducing the risk of burnout. In specialties like internal medicine and family practice, where visit volumes are high, this efficiency directly translates into improved productivity, better compliance, and higher-quality notes.
4. Optimized Medical Research and Drug Development
AI is accelerating the pace of clinical research by identifying patient cohorts, simulating drug responses, and analyzing trial data in real-time. In pharmacology, platforms like BenevolentAI and Insilico Medicine are using deep learning to identify novel drug targets and predict molecule behavior, shortening the drug development lifecycle.
Clinical trial matching is also becoming more efficient. AI systems rapidly sift through electronic health records to find eligible patients based on highly specific inclusion criteria. This improves trial recruitment timelines and ensures that investigational therapies reach the right patient populations faster.
5. Improved Diagnostic Consistency Across Specialties
AI reduces inter-physician variability in diagnosis by providing standardized interpretations of clinical data. In dermatology, AI tools trained on millions of skin images now diagnose melanoma with accuracy on par with expert dermatologists. In ophthalmology, algorithms can detect diabetic retinopathy from retinal scans with high sensitivity and specificity.
This consistency is particularly valuable in under-resourced settings or when specialist access is limited. AI acts as a clinical second opinion, reducing the rate of misdiagnosis and helping general practitioners manage complex cases more confidently and accurately.
Challenges Facing AI Adoption in Medicine
Despite its clinical potential, AI adoption in medicine faces significant hurdles that limit reliability, trust, and long-term scalability. These challenges go beyond technical constraints; they involve data integrity, physician confidence, regulatory oversight, and clinical workflow alignment.

1. Fragmented and Poor-Quality Clinical Data
AI models rely on large volumes of structured and unstructured medical data, such as lab results, imaging, genomic profiles, clinical notes, but this data is often incomplete, siloed, or inconsistently formatted. Variability in diagnostic coding, missing lab values, and incompatible imaging standards can undermine model performance.
Solving this issue requires more than technical integration. It demands standardized data entry, interoperability between EHR systems, and active clinician involvement in data stewardship. Until these gaps are addressed, AI systems in medicine will struggle to deliver consistent or clinically reliable insights.
2. Limited Clinical Validation and Generalizability
Many AI tools are trained on narrow or institution-specific datasets, which limits their ability to generalize across diverse patient populations or practice environments. A model that performs well in one academic center may underperform in a rural hospital or among underrepresented populations.
Without prospective validation in varied real-world settings, clinicians may hesitate to rely on AI outputs. Regulatory bodies are also increasingly requiring broader validation before clinical deployment. Ensuring reproducibility across contexts is essential for trust and adoption.
3. Regulatory Uncertainty and Liability Concerns
The regulatory landscape for AI in medicine remains fragmented. While the FDA has cleared several AI-based diagnostic tools, there is no unified framework for adaptive or continuously learning algorithms. Clinicians may be unclear on who holds liability when AI errors occur.
Until clearer guidance emerges, physicians may underuse AI tools, especially in high-risk specialties like oncology or cardiology. Transparent risk stratification, explainability features, and collaborative regulation are needed to clarify responsibility and build clinician trust.
4. Overreliance and Skill Degradation
AI tools can streamline diagnosis and decision-making, but excessive reliance may erode physician diagnostic acumen over time. A recent study in gastroenterology found that routine AI assistance during colonoscopies led to decreased detection performance when AI was turned off.
To mitigate this, clinicians must remain engaged as decision-makers, not passive recipients of AI suggestions. Institutions should implement AI as an augmentative tool with regular assessments and training to maintain clinical skills and oversight.
5. Bias and Inequity in Medical AI
AI models can inadvertently reflect and reinforce existing disparities in medicine. If training data underrepresents certain ethnicities, ages, or comorbidities, the model’s recommendations may be less accurate or even harmful for those populations.
This is especially dangerous in specialties like dermatology, where skin conditions present differently across skin tones. Mitigating bias requires diverse, representative training datasets and continuous bias auditing. Without this, AI may amplify, rather than correct, inequities in care.
Specific Applications of AI in Medicine
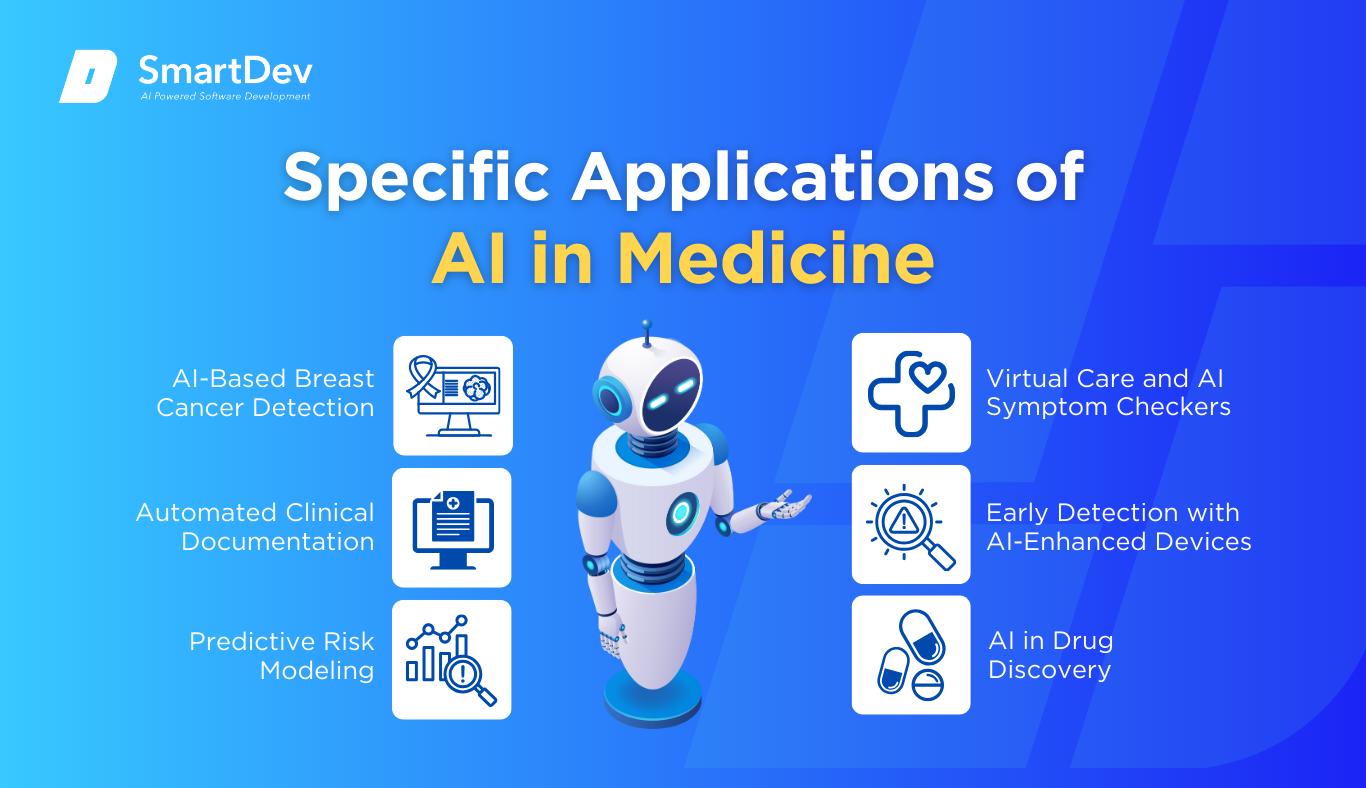
1. AI-Based Breast Cancer Detection
AI-based breast cancer detection enhances early diagnosis by analyzing mammogram images for suspicious patterns with high accuracy. These systems leverage deep learning, particularly convolutional neural networks (CNNs), trained on vast datasets of annotated mammograms. They assist radiologists by flagging regions of interest and prioritizing high-risk cases for immediate review.
The models operate by identifying microcalcifications, masses, and architectural distortions indicative of malignancy. Integration into clinical imaging systems allows for real-time support during screenings, reducing diagnostic delays. This approach increases sensitivity, reduces false negatives, and offers consistency across patient demographics.
Google Health developed an AI system that outperformed human radiologists in detecting breast cancer from mammograms. In a large-scale study published in Nature, the AI reduced false positives by 5.7% and false negatives by 9.4% compared to expert radiologists. The tool is being evaluated for integration into national screening programs in the UK and U.S.
2. Automated Clinical Documentation
AI-based medical scribes are transforming how clinicians document patient encounters by automating the transcription and summarization of doctor-patient conversations. Using large language models, these systems capture key details in real-time and generate structured notes that integrate into the electronic health record (EHR). This reduces administrative workload and allows doctors to focus more on patient care.
The AI systems process audio recordings, apply natural language understanding (NLU) to extract clinical terms, and generate compliant documentation that adheres to hospital formats. Most tools integrate with existing EHR platforms, ensuring seamless clinical workflows. Benefits include reduced clinician burnout, improved note accuracy, and increased patient face-time.
Clinics in the UK using ambient AI scribes reported time savings and higher satisfaction, with 80% of general practitioners noting improved efficiency. The tools captured notes during patient visits and automatically entered them into EHR systems. This reduced after-hours charting and enhanced the doctor-patient relationship.
3. Predictive Risk Modeling
Predictive analytics in medicine enables early identification of patients at risk for adverse events such as sepsis, readmissions, or disease progression. AI models analyze EHR data, lab results, and clinical histories to flag high-risk individuals and trigger preventive measures. This proactive care improves patient outcomes and reduces healthcare costs.
The underlying models often use decision trees, gradient boosting, or neural networks trained on longitudinal patient data. They continuously monitor new data points and adjust risk scores in real-time, alerting care teams for follow-up. These systems are embedded in clinical workflows and EHR dashboards.
More than 65% of U.S. hospitals use AI predictive models for inpatient care management. For example, models flag patients likely to deteriorate, enabling earlier intervention. Hospitals report fewer ICU transfers and shorter lengths of stay as a result.
4. Virtual Care and AI Symptom Checkers
Virtual care platforms enhanced by AI provide around-the-clock triage and symptom assessment for patients. These tools use conversational interfaces to gather symptom information and suggest possible conditions or care steps. They reduce unnecessary clinic visits and improve care accessibility.
AI models are trained on large datasets of symptom-condition pairs, and use probabilistic reasoning and natural language processing to assess input data. Many systems connect to EHRs and escalate urgent cases to clinicians. This creates a hybrid care model that combines automation with human oversight.
Cedars-Sinai’s CS Connect platform has handled over 42,000 patient sessions using an AI engine developed with K Health. The system delivered treatment recommendations rated as optimal 77% of the time compared to 67% from physicians. This improved efficiency while maintaining high-quality care.
5. Early Detection with AI-Enhanced Devices
AI-powered diagnostic tools such as smart stethoscopes help identify diseases like arrhythmias or heart valve disorders in real-time. These devices analyze physiological signals using AI models to detect abnormal patterns during routine exams. This allows for earlier detection and intervention, even in primary care settings.
The devices utilize embedded sensors and AI algorithms trained on annotated heart or lung sounds, and some also process ECG signals. Clinicians receive immediate feedback and risk scores through companion mobile apps or devices. These tools are especially useful in resource-constrained environments.
At Imperial College, researchers created a stethoscope that diagnoses heart issues in 15 seconds. Despite its accuracy, 70% of users stopped using it within a year due to integration challenges. The device showed potential but highlighted the need for user-centered design.
6. AI in Drug Discovery
AI is streamlining drug discovery by predicting drug-target interactions, screening compounds, and modeling drug efficacy. These tools help pharmaceutical companies identify promising molecules faster and reduce the cost of R&D. They’re especially useful in oncology, rare diseases, and infectious disease domains.
The platforms combine bioinformatics, cheminformatics, and machine learning to analyze vast datasets of molecular structures and biological responses. Some systems generate synthetic compounds, while others identify new uses for existing drugs. Integration with laboratory automation accelerates the pipeline.
Eli Lilly launched TuneLab, an AI-powered drug discovery initiative collaborating with startups like Circle Pharma. These partnerships leverage AI models to develop targeted therapies more efficiently. Early outcomes show accelerated timelines and improved compound viability.
Need Expert Help Turning Ideas Into Scalable Products?
Partner with SmartDev to accelerate your software development journey — from MVPs to enterprise systems.
Book a free consultation with our tech experts today.
Let’s Build TogetherExamples of AI in Medicine
AI adoption in medicine is no longer experimental; it’s operational. From predictive diagnostics to virtual care delivery, real-world deployments prove how AI can elevate outcomes and optimize the full spectrum of clinical workflows.
Real-World Case Studies

1. Cleveland Clinic: AI for Cardiac MRI Analysis
Cleveland Clinic partnered with an AI startup to automate the interpretation of cardiac MRI scans, reducing analysis time from hours to minutes. The AI software segments the heart’s anatomy and calculates ejection fraction, wall thickness, and perfusion in real time. This enhances diagnostic precision and reduces inter-observer variability in cardiology assessments.
The tool was integrated into their imaging workflow and validated against expert radiologist benchmarks. Since implementation, the clinic reported a 60% reduction in report turnaround time. It also improved early detection rates of conditions like hypertrophic cardiomyopathy and heart failure.
2. Mount Sinai Health System: AI for Stroke Detection
Mount Sinai integrated AI-based imaging software into its stroke care units to accelerate the detection of large vessel occlusions from CT angiograms. The system analyzes scans in under two minutes, alerting neurovascular teams in real-time to initiate rapid response protocols. This reduced the door-to-treatment time for stroke patients and improved outcomes in critical care cases.
Their platform, powered by Viz.ai, leverages deep learning and cloud-based communication to streamline interdepartmental collaboration. Since deployment, Mount Sinai reported a 40% reduction in door-to-needle time and improved patient discharge rates. The AI tool has become a core component of their time-sensitive emergency workflows.
3. Novartis: Accelerating Drug Development with AI
Novartis has deployed AI across its drug development pipeline to optimize candidate molecule selection and improve clinical trial design. By analyzing biomedical literature, genomics data, and clinical outcomes, the AI system identifies promising compounds and predicts efficacy and safety profiles. This data-driven approach helps reduce R&D costs and speeds up time-to-market.
The company partners with Microsoft and uses platforms like Project DataSphere and Synthego’s CRISPR datasets to train models. In recent oncology trials, AI reduced compound screening time by 50% and increased success rates in early-phase trials. Novartis considers AI a strategic asset for maintaining competitiveness in precision medicine.
4. NHS Chelsea: AI Skin Cancer Screening
The NHS at Chelsea and Westminster Hospital implemented an AI-powered mobile app that assesses skin lesions using smartphone photos. Patients receive near-instant feedback on potential skin cancer risks, allowing high-risk cases to be escalated while providing peace of mind to low-risk individuals. This has significantly improved access to dermatological screening.
The tool uses deep learning algorithms trained on over 1 million images to classify lesions with high accuracy. Over 13,000 confirmed skin cancers have been detected through the app since launch. Screening time dropped from 20 minutes to under 5 minutes, easing the burden on dermatology departments.
Innovative AI Solutions
AI-Driven Innovations Transforming Medicine
Emerging Technologies in AI for Medicine

Generative AI is redefining how medical professionals diagnose, treat, and manage patient care. These tools are powering drug discovery, synthesizing clinical trial data, and generating personalized care plans. In biotech, companies can generative models to design entirely new molecules, dramatically cutting down the time and cost of traditional R&D. In clinical settings, AI scribes are relieving doctors of the burden of note-taking, allowing more time for patient interaction and decision-making.
Computer vision is transforming medical diagnostics. AI algorithms now outperform humans in reading radiographs, detecting tumors, and analyzing skin lesions. In the UK, NHS hospitals use computer vision tools to analyze mammograms and detect breast cancer with higher sensitivity—sometimes identifying abnormalities missed by radiologists. In dermatology, smartphone apps equipped with vision models can now evaluate moles or rashes with near-clinical accuracy, making early intervention accessible even in remote areas.
Agentic AI is emerging as a game-changer across hospital systems. These autonomous agents can triage patients, analyze vitals, and suggest care pathways—without requiring constant supervision. At Cedars-Sinai, intelligent agents embedded in digital front doors handle intake, answer questions, and schedule follow-ups. These AI systems free up valuable clinical staff, enabling them to focus on complex care delivery while ensuring patients stay engaged and informed throughout their medical journey.
AI’s Role in Sustainability Efforts
AI is helping medical systems operate smarter and leaner—something every hospital administrator is aiming for. Predictive analytics now guide everything from emergency department staffing to ICU bed management. Hospitals are leveraging AI to forecast patient admissions and length of stay, which means they can allocate staff and equipment more efficiently, avoid unnecessary testing, and reduce readmissions.
On the infrastructure side, AI is powering energy-efficient smart hospitals. Facilities use machine learning to regulate temperature, optimize lighting, and monitor equipment usage in real time. These systems adjust dynamically based on occupancy patterns and medical device load, slashing energy consumption without compromising safety or care quality.
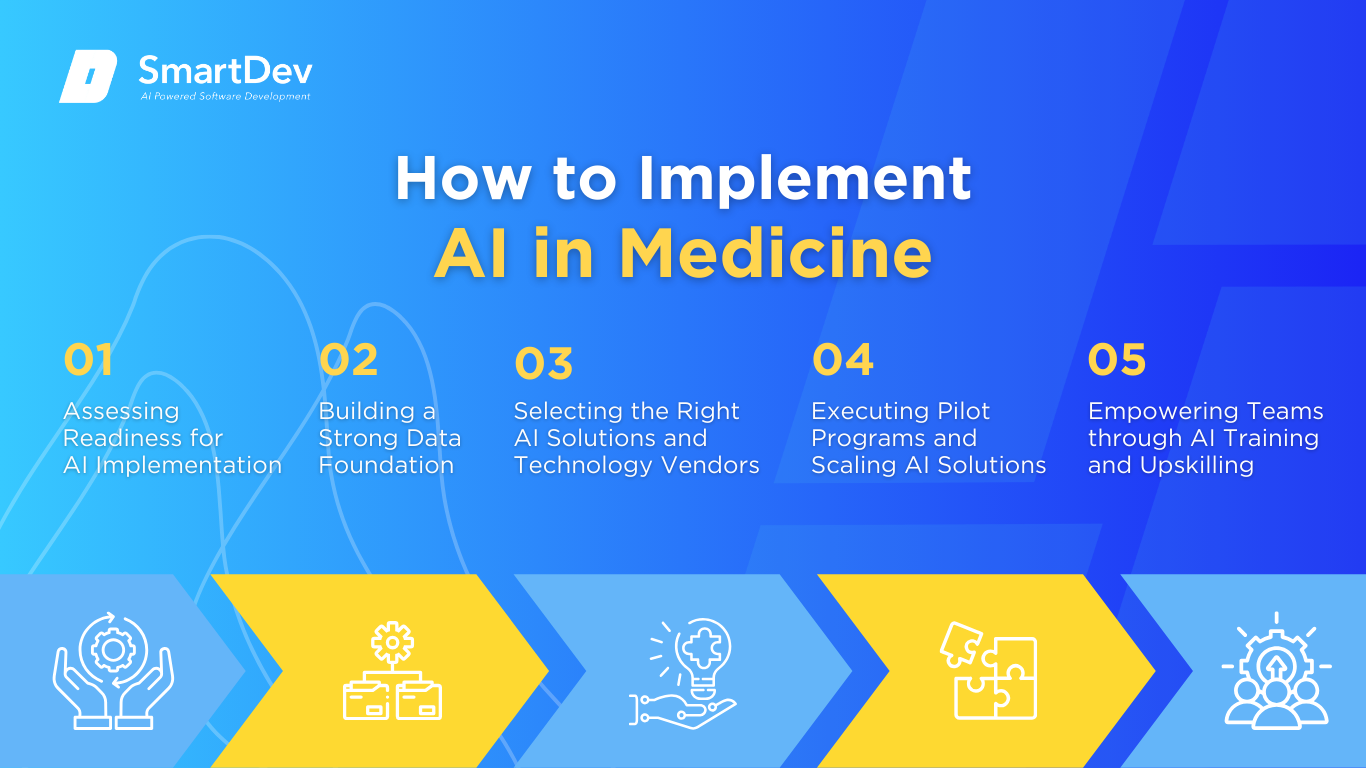
How to Implement AI in Medicine
Step 1: Assessing Readiness for AI Adoption
Before jumping into AI, medical organizations need to identify where it can make the biggest impact. Common entry points include imaging diagnostics, clinical documentation, patient triage, and operational forecasting. These areas are often repetitive and data-driven—ideal for AI assistance.
Readiness also requires more than just technology. Evaluate your IT infrastructure, leadership alignment, and digital maturity. Are your systems interoperable? Are your teams open to innovation? Running a readiness audit early helps set realistic expectations, uncover technical gaps, and align stakeholders around clear outcomes.
Step 2: Building a Strong Data Foundation
AI is only as effective as the data it’s built on. In medicine, that means clinical records must be structured, accurate, and complete. Disorganized EHRs, inconsistent terminology, and siloed data will undermine AI outcomes before they even start.
Invest in data cleaning, standardization, and governance. Engage clinicians in defining what clean, usable data looks like from a practical perspective. When your foundation is solid, AI tools can deliver meaningful insights that actually support clinical decision-making.
Step 3: Choosing the Right Tools and Vendors
Choosing an AI tool for medicine isn’t about finding the flashiest tech—it’s about fit. Look for platforms that are proven in real clinical settings, have regulatory clearance, and can integrate directly with your existing systems without disruption.
Also consider long-term scalability and support. The best vendors act like partners, not just providers. They offer onboarding, training, and transparency around model performance. If they can’t explain how their AI works in your context, they’re not the right fit.
Step 4: Pilot Testing and Scaling Up
AI should be tested just like any clinical intervention. Start with a small-scale pilot—such as AI-powered note-taking in outpatient visits or triage automation in emergency departments. Define success metrics early and collect feedback from front-line users.
Once results are consistent, scale gradually. Use what you learn to fine-tune workflows and adjust training. Pilots also help build trust internally—seeing real ROI in one department makes it easier to expand system-wide adoption.
Step 5: Training Teams for Successful Implementation
AI doesn’t replace clinicians, it augments them. But to make that happen, your teams need to understand what AI does, how it fits into their workflow, and where human judgment still matters most.
Training should go beyond tool usage. Create a culture of AI literacy that empowers your staff to question, validate, and collaborate with AI. When clinicians feel informed and supported, they’re more likely to trust the technology and use it to deliver safer, faster, and better care.
Measuring the ROI of AI in Medicine
Key Metrics to Track Success
Assessing AI’s return on investment in medicine is about how it improves care delivery, operational flow, and patient outcomes. Start with productivity gains: measure how much faster clinicians complete documentation, how many more scans radiologists can interpret, or how autonomously chronic disease management has improved. Comparing before-and-after data in these areas provides clear evidence of efficiency and capacity gains.
Next, quantify cost savings, from reduced overtime when documentation is automated, to fewer unnecessary tests thanks to accurate triage. For instance, AI that accelerates stroke detection can shorten hospital stays, reduce resource strain, and cut follow-up costs. The administrative lift that’s eliminated translates directly into financial savings.
Finally, don’t underestimate patient-focused outcomes. Early detection tools that increase diagnostic accuracy or predictive models that reduce hospital readmissions deliver both care quality and long-term financial value. Plus, higher patient satisfaction can boost outcome-based reimbursements—making AI not just a tool, but a way to enhance fiscal resilience.
Case Studies Demonstrating ROI
Consider a radiology department that implemented AI for lung nodule detection. Within months, radiologists could interpret 25% more CT scans daily, while maintaining diagnostic accuracy—effectively expanding capacity without hiring or overtime.
In another case, a community clinic adopted an AI scribe to handle charting. Physicians reported a 50% reduction in after-hours documentation time. That time savings translated into fewer burnout symptoms, higher job satisfaction, and better staff retention.
An emergency unit using AI-assisted triage software cut decision-to-treatment time by nearly 30%. Faster interventions led to shorter hospital stays, fewer complications, and measurable drops in inpatient costs. These real-world gains illustrate how medicine-focused AI converts into both clinical and financial value.
Common Pitfalls and How to Avoid Them
One frequent mistake is launching AI projects without anchoring them to concrete clinical problems. Ambitious tools that solve non-urgent issues often disappoint. Begin every AI initiative with a clear challenge, defined success measures, and an explicit hypothesis about where value will come.
Data quality remains a major barrier. If your medical data is incomplete, inconsistent, or siloed, AI outputs risk being misleading—and your clinical team will lose trust fast. Prioritize data standardization, privacy safeguards, and quality audits throughout the implementation lifecycle.
Equally important is staff acceptance. Without clinician buy-in, even the best AI can fail. Counter skepticism by being transparent, educating teams, and celebrating early wins that show how AI complements their work. When AI earns trust, ROI follows.
Future Trends of AI in Medicine

Predictions for the Next Decade
In the coming decade, AI will evolve from supporting clinical tasks to orchestrating entire patient journeys, from pre-diagnosis screening to recovery monitoring. AI won’t just flag abnormalities or automate paperwork; it will recommend treatment paths, coordinate multi-specialty care, and even adjust care plans in real time based on new data.
We’ll also see deeper integration between AI and connected devices. Wearables, implantables, and home-based monitoring systems will feed continuous data to medical AI systems, allowing conditions like heart failure, diabetes, or even post-operative recovery to be tracked proactively outside the hospital. This shift will reduce hospital readmissions and make precision medicine truly scalable.
Meanwhile, LLMs trained on medical literature and patient records will evolve into clinical co-pilots—fluent in diagnostics, care coordination, and medical reasoning. These models will move beyond task automation toward context-aware decision-making, transforming how care is delivered, especially in time-critical or resource-limited settings.
How Businesses Can Stay Ahead of the Curve
To lead in this AI-powered future, healthcare organizations must stop treating AI as a side project and start embedding it into their core strategy. That means aligning leadership vision, clinical workflows, and digital infrastructure with a shared AI roadmap that focuses on long-term transformation.
Building in-house AI literacy and forming strategic partnerships will be essential. Whether you collaborate with research labs, tech startups, or health AI consortiums, staying connected to the innovation ecosystem ensures you’re not left behind. Modular, interoperable systems will give you flexibility as AI technologies continue to evolve.
Above all, cultivate a culture where experimentation is safe, data is respected, and clinicians feel empowered by automation. Organizations that treat AI as a strategic collaborator, not just a tool, will be the ones reshaping the next era of modern medicine.
Conclusion
Key Takeaways
AI is reshaping medicine by improving diagnostic accuracy, streamlining workflows, and enabling earlier, more personalized interventions. From ambient clinical documentation to imaging interpretation, risk prediction, and care coordination, AI is no longer experimental—it’s foundational to the future of modern medicine.
Healthcare organizations that build strong data foundations, prioritize high-impact use cases, and foster a culture of AI fluency are already realizing measurable gains in clinical efficiency, cost reduction, and patient satisfaction. As AI shifts from automating tasks to managing entire care pathways, its ability to adapt in real time and scale across departments will define the next wave of clinical excellence.
Medicine is at a turning point. The decisions you make today, around infrastructure, partnerships, and organizational readiness, will determine whether your system thrives in an AI-driven future or struggles to keep up.
Moving Forward: A Strategic Approach to AI in Medicine
If you’re ready to lead the next generation of care delivery, now is the time to approach AI strategically. Identify the medical functions where AI can deliver the most impact—whether that’s improving imaging turnaround times, reducing clinician burnout, or expanding access in underserved regions. Build a secure, clean, and scalable data infrastructure, and choose technology partners who understand the complexity and responsibility of healthcare.
At SmartDev, we collaborate with hospitals, clinics, and healthcare innovators to turn AI potential into clinical reality. From selecting the right tools and launching targeted pilots to training your staff and measuring ROI, we help you build AI solutions that are practical, compliant, and aligned with patient care goals.
The future of medicine is intelligent, adaptive, and data-driven. Let’s shape it together.
—
References:
- AI Applications in Healthcare: Opportunities, Challenges, and Ethical Considerations | PMC
- 65 Key AI in Healthcare Statistics | TempDev
- New AMA Report Highlights Physician Optimism About AI in Healthcare | Medical Economics
- London Hospital Uses AI for Skin Cancer Checks | Evening Standard
- Novartis Empowers Scientists with AI to Speed Discovery of Breakthrough Medicines | Microsoft Transform
- Mount Sinai’s AI Model May Shift Stroke Care | Becker’s Hospital Review
- AI Tool Improves Cardiac Amyloidosis Diagnosis via MRI | Cleveland Clinic Consult QD
- Lilly Launches Tunelab Platform for AI-Enabled Drug Discovery | Life Science History
- How AI Helped Cedars-Sinai Deliver Faster, Smarter Patient Care | Apoio.ai
- Google Health: Advancing AI in Mammography | Google Health